The aim of our study was to investigate the causes of fetal growth <10th centile diagnosed <26 weeks’ gestation in singleton pregnancies and compare pregnancy outcomes in relation to the identified etiology.
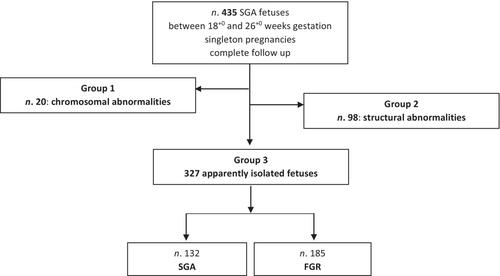
Historical cohort study conducted in two Italian hospitals which included all small-for-gestational-age fetuses diagnosed between 18+0 and 26+0 weeks over a 10-year period. Fetuses were divided into three groups depending on the prenatally suspected etiology: chromosomal abnormalities (Group 1), malformations (Group 2) and isolated (Group 3). These groups were compared regarding pregnancy outcomes. Fetuses in Group 3 were divided into small-for-gestational-age and fetal growth restriction following the Delphi Consensus criteria and the outcomes were further compared. Fisher's Exact or Mann–Whitney test were used for comparison of groups.
In all, 435 fetuses were included. Of these, 20 cases (4.6%) were associated with chromosomal abnormalities (Group 1), 98 (22.5%) with fetal malformations (Group 2) and 317 (72.9%) were isolated (Group 3). A higher percentage of live births was reported for Group 3 (P < 0.001). Termination of pregnancy was more common in Group 1 (P < 0.001). No differences in gestational age at delivery, birthweight, intrauterine death or neonatal death were detected within groups. Growth-restricted fetuses had lower gestational age at delivery, birthweight and number of live births (P < 0.001), higher rates of termination of pregnancy, intrauterine death (P < 0.001) and neonatal death <10 days (P = 0.002) compared to small-for-gestational-age. In 17 cases a chromosomal abnormality, genetic syndrome or adverse neurological outcome was diagnosed after birth: six from Group 2 (11.3% of live births in this group) and 11 from Group 3 (4.3%).
We report that fetal growth <10th percentile diagnosed before 26 weeks is not isolated before birth in 27% of cases. Malformations and chromosomal abnormalities are common etiologies; therefore, detailed anomaly scans and invasive testing should be offered. In addition, there is a residual risk of neonatal death and postnatal diagnosis of a genetic syndrome or neurodevelopmental impairment despite normal prenatal tests. These results expand the small amount of information on the outcome of cases with very early diagnosis of impaired fetal growth currently available and highlight the importance of detailed counseling with couples.