Soft tissue trunk reconstruction is often challenging. Although free microvascular flaps are a feasible option in case of extensive defects involving deep structures, pedicled flaps represent a good alternative, especially if harvested and dissected with a “microsurgical” approach. The aim of this study is to evaluate the feasibility of trunk reconstruction with the use of pedicled flaps, according to the application of our reconstructive algorithm, and to compare it to other reconstructive methods.
From January 2017 to December 2021, we retrospectively analyzed patients who underwent soft tissue reconstruction of the trunk with pedicled flaps at the authors' institution. Patient's demographic, clinical and surgical characteristics and postoperative complications were recorded and analyzed by descriptive statistics. A comparative analysis was made between the study group and two other groups who underwent reconstruction of trunk defects with free flaps and skin grafts, respectively, at the authors' institution.
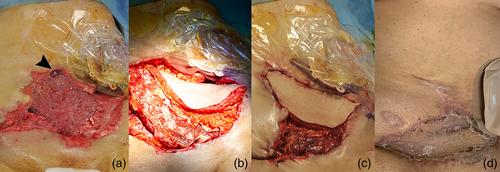
Forty-seven patients were included in the study. Patients' age ranged between 36 and 82 years (mean: 57.8 years). Twenty-eight patients were male, while 19 patients were female. In 76.6% of patients (36 out of 47), reconstructive procedures were performed to repair defects resulting from cancer resection. Reconstruction of superficial defects was always achieved with perforator flaps (n = 25). In case of full-thickness defects, reconstruction was carried out with musculocutaneous flaps (n = 22); latissimus dorsi and vastus lateralis were the most used flaps for chest and abdominal wall reconstruction, respectively. In our series, we observed only one case of total flap loss requiring re-operation under general anesthesia. Minor complications occurred in 8.5% of cases (4 out of 47 patients). We observed two cases of partial flap necrosis and two cases of wound dehiscence. In the skin grafts group (n = 53), the mean age was 54.5 years (range 39–85) and 56% of patients were male (n = 30). In 66% of cases (n = 30) the defect resulted from oncological resection. The overall complication rate was 18.8% (n = 10). In the free flaps group (n = 10), the mean age was 49.0 years (range 29–77) and 60% of patients (n = 6) were male. In 70% of cases (n = 7) the defect was caused by oncological resection. Complications occurred in two patients (20%).
No statistically significant differences were found in terms of overall complication rate between the study group and the two comparative groups (p = .48). A significant correlation was found between the reconstructive method and the type and size of the defect, with reconstruction through free flaps being associated with larger (344.0 vs. 220.4 cm2) (p = .04) and full-thickness defects (80.0% vs. 46.8%) (p < .01) if compared to pedicled flaps.
In the new era of microsurgery, pedicled flaps represent a valid alternative to free flaps for the majority of soft tissue defects of the trunk. In our series, no statistically significant differences in terms of complications were found between reconstructions of similar defects achieved with pedicled and free flaps, and free flap use was limited to extensive full-thickness defects. In addition, the rate of postoperative complications with pedicled flaps found in our cohort was lower than the rate reported in the literature.