A multidisciplinary approach is the gold standard in the management of persistent pain and is current practice in tertiary pain clinics. However, such approaches seem to be a rarity in primary care, although pain is the most common reason for visiting a primary care physician. A comprehensive systematic review was conducted to explore whether studies on multidisciplinary management programs for persistent pain exist in primary care.
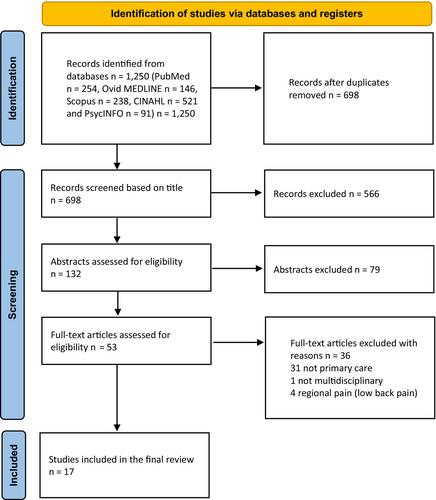
PubMed, Ovid MEDLINE, Scopus, CINAHL, and PsychINFO were searched from inception to October 2022, and supplementary research was conducted in June 2023. Screening, data extraction, and quality assessment were independently carried out by two researchers. The inclusion criteria were (1) adult patients (age >18 years); (2) non-cancer pain, persisting over 3 months; (3) multidisciplinary intervention (treatment included ≥3 heathcare professionals); (4) intervention conducted in a primary care setting; and (5) reports published in English.
Of the 1250 initially identified studies, 17 were selected for final analysis. Only studies reporting empirical data were included (cohort, case–control, randomized controlled trial, and observational). The study settings and intervention characteristics showed great heterogeneity. The primary care practices also varied across different countries and cultures. Overall, the quality of the studies was rather low and sample sizes were relatively small.
The review revealed that studies about such treatment interventions for persistent pain patients are scarce. The existing studies were heterogeneous in terms of intervention characteristics, population, outcome variables, and study methodology. Future studies are urgently needed.
Persistent pain is a growing challenge to the health care system, and most patients are treated in primary care. The biopsychosocial concept is the basis for the multidisciplinary management of pain. The review revealed that studies about treatment interventions for persistent pain patients are scarce. Existing studies were heterogeneous in terms of intervention characteristics, population, outcome variables, and study methodology. There is an urgent need for further studies on systematic multidisciplinary treatment protocols for managing persistent pain in primary care.