Gene therapy with AAV9-SGPL1 in an animal model of lung fibrosis
Aritra Bhattacharyya, Ranjha Khan, Joanna Y Lee, Gizachew Tassew, Babak Oskouian, Maria L Allende, Richard L Proia, Xiaoyang Yin, Javier G Ortega, Mallar Bhattacharya, Julie D Saba
下载PDF
{"title":"Gene therapy with AAV9-SGPL1 in an animal model of lung fibrosis","authors":"Aritra Bhattacharyya, Ranjha Khan, Joanna Y Lee, Gizachew Tassew, Babak Oskouian, Maria L Allende, Richard L Proia, Xiaoyang Yin, Javier G Ortega, Mallar Bhattacharya, Julie D Saba","doi":"10.1002/path.6256","DOIUrl":null,"url":null,"abstract":"<p>Idiopathic pulmonary fibrosis (IPF) is a progressive scarring disease of the lung that leads rapidly to respiratory failure. Novel approaches to treatment are urgently needed. The bioactive lipid sphingosine-1-phosphate (S1P) is increased in IPF lungs and promotes proinflammatory and profibrotic TGF-β signaling. Hence, decreasing lung S1P represents a potential therapeutic strategy for IPF. S1P is degraded by the intracellular enzyme S1P lyase (SPL). Here we find that a knock-in mouse with a missense SPL mutation mimicking human disease resulted in reduced SPL activity, increased S1P, increased TGF-β signaling, increased lung fibrosis, and higher mortality after injury compared to wild type (WT). We then tested adeno-associated virus 9 (AAV9)-mediated overexpression of human <i>SGPL1</i> (AAV-SPL) in mice as a therapeutic modality. Intravenous treatment with AAV-SPL augmented lung SPL activity, attenuated S1P levels within the lungs, and decreased injury-induced fibrosis compared to controls treated with saline or only AAV. We confirmed that AAV-SPL treatment led to higher expression of SPL in the epithelial and fibroblast compartments during bleomycin-induced lung injury. Additionally, AAV-SPL decreased expression of the profibrotic cytokines TNFα and IL1β as well as markers of fibroblast activation, such as fibronectin (<i>Fn1</i>), <i>Tgfb1</i>, <i>Acta2</i>, and collagen genes in the lung. Taken together, our results provide proof of concept for the use of AAV-SPL as a therapeutic strategy for the treatment of IPF. © 2024 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"263 1","pages":"22-31"},"PeriodicalIF":5.6000,"publicationDate":"2024-02-09","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6256","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6256","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
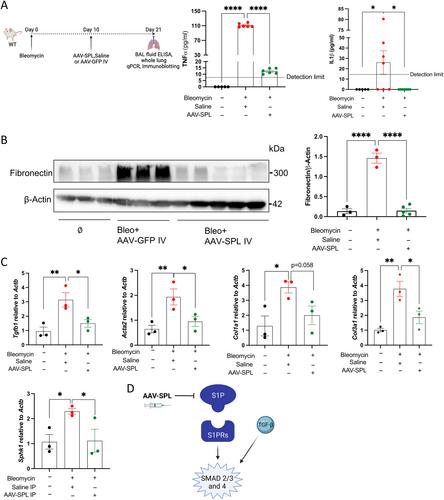
Idiopathic pulmonary fibrosis (IPF) is a progressive scarring disease of the lung that leads rapidly to respiratory failure. Novel approaches to treatment are urgently needed. The bioactive lipid sphingosine-1-phosphate (S1P) is increased in IPF lungs and promotes proinflammatory and profibrotic TGF-β signaling. Hence, decreasing lung S1P represents a potential therapeutic strategy for IPF. S1P is degraded by the intracellular enzyme S1P lyase (SPL). Here we find that a knock-in mouse with a missense SPL mutation mimicking human disease resulted in reduced SPL activity, increased S1P, increased TGF-β signaling, increased lung fibrosis, and higher mortality after injury compared to wild type (WT). We then tested adeno-associated virus 9 (AAV9)-mediated overexpression of human SGPL1 (AAV-SPL) in mice as a therapeutic modality. Intravenous treatment with AAV-SPL augmented lung SPL activity, attenuated S1P levels within the lungs, and decreased injury-induced fibrosis compared to controls treated with saline or only AAV. We confirmed that AAV-SPL treatment led to higher expression of SPL in the epithelial and fibroblast compartments during bleomycin-induced lung injury. Additionally, AAV-SPL decreased expression of the profibrotic cytokines TNFα and IL1β as well as markers of fibroblast activation, such as fibronectin (Fn1 ), Tgfb1 , Acta2 , and collagen genes in the lung. Taken together, our results provide proof of concept for the use of AAV-SPL as a therapeutic strategy for the treatment of IPF. © 2024 The Authors. The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
在肺纤维化动物模型中使用 AAV9-SGPL1 进行基因治疗。
特发性肺纤维化(IPF)是一种进行性肺部瘢痕疾病,会迅速导致呼吸衰竭。目前迫切需要新的治疗方法。生物活性脂质鞘氨醇-1-磷酸酯(S1P)在 IPF 肺中增加,并促进促炎和促坏死性 TGF-β 信号传导。因此,减少肺部 S1P 是治疗 IPF 的一种潜在策略。S1P由细胞内的S1P裂解酶(SPL)降解。在这里,我们发现,与野生型(WT)相比,具有模拟人类疾病的SPL错义突变的基因敲入小鼠会导致SPL活性降低、S1P增加、TGF-β信号传导增加、肺纤维化加重以及损伤后死亡率升高。我们随后测试了由腺相关病毒 9(AAV9)介导的小鼠过表达人 SGPL1(AAV-SPL)的治疗方法。与用生理盐水或仅用 AAV 治疗的对照组相比,AAV-SPL 静脉治疗增强了肺 SPL 活性,降低了肺内 S1P 水平,并减少了损伤引起的纤维化。我们证实,在博莱霉素诱导的肺损伤过程中,AAV-SPL 处理可导致上皮细胞和成纤维细胞中 SPL 的高表达。此外,AAV-SPL 还降低了肺部组织坏死细胞因子 TNFα 和 IL1β 的表达,以及成纤维细胞活化的标志物,如纤维连接蛋白 (Fn1)、Tgfb1、Acta2 和胶原基因。综上所述,我们的研究结果为使用 AAV-SPL 作为治疗 IPF 的治疗策略提供了概念证明。© 2024 作者。病理学杂志》由约翰威利父子有限公司代表大不列颠及爱尔兰病理学会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。