People with high blood pressure have reduced sensitivity to pain, known as blood pressure hypoalgesia. One proposed mechanism for this is altered baroreceptor sensitivity. In healthy volunteers, stimulating the carotid baroreceptors causes reduced sensitivity to acute pain; however, this effect may be confounded by a rise in blood pressure due to baroreflex stimulation. The present study tests whether baroreceptor unloading contributes to the physiological mechanism of blood pressure-related hypoalgesia.
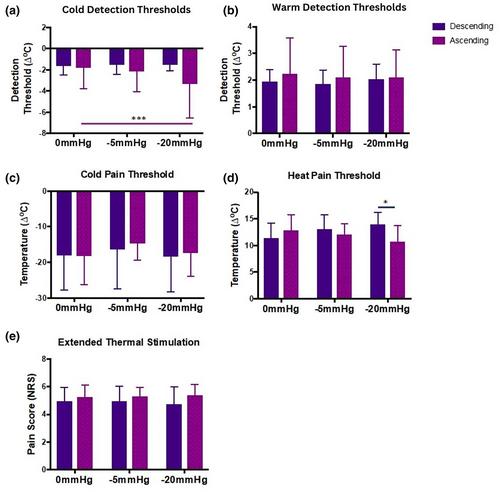
In the present study, pain perception to thermal stimulation of the forearm was studied in 20 healthy volunteers during baroreceptor unloading by lower body negative pressure (LBNP) at −5 and −20 mmHg. Blood pressure and heart rate were measured continuously throughout. To address issues relating to stimulation order, the sequence of LBNP stimulation was counterbalanced across participants.
Increased heart rate was observed at a LBNP of −20 mmHg, but not −5 mmHg, but neither stimulus had an effect on blood pressure. There was no change in warm or cold sensory detection thresholds, heat or cold pain thresholds nor perceived pain from a 30s long thermal heat stimulus during LBNP.
Therefore, baroreceptor unloading with maintained systemic blood pressure did not alter pain perception. The current study does not support the hypothesis that an altered baroreflex may underlie the physiological mechanism of blood pressure-related hypoalgesia.
This work provides evidence that, when measured in normotensive healthy young adults, the baroreflex response to simulated hypovolaemia did not lead to reduced pain sensitivity (known as blood pressure hypoalgesia).