To evaluate the effectiveness of optical coherence tomography angiography (OCTA) in detecting early intraocular microvascular changes in diabetic patients.
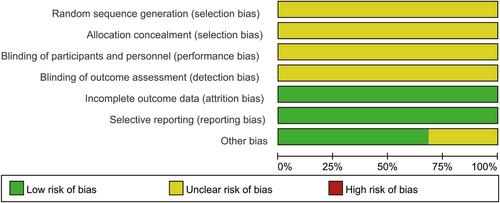
A systematic study search was performed on PubMed, Medline, Embase, and the Cochrane Library, ranging from January 2012 to March 2023. Controlled studies compared diabetes mellitus (DM) patients with non-diabetic retinopathy (NDR) or patients with mild non-proliferative diabetic retinopathy (mild NPDR) to healthy people. These studies included parameters of OCTA such as foveal avascular zone (FAZ), vessel density of superficial capillary plexus (VDscp), vessel density of deep capillary plexus (VDdcp), and peripapillary VD. The relevant effect model was used according to the heterogeneity, and the mean difference and 95% confidence intervals were calculated.
A total of 18 studies with 2101 eyes were eventually included in this meta-analysis. Our results demonstrated that early alterations of VDscp, VDdcp, and peripapillary VD in NDR patients had a significant difference compared with healthy people by OCTA (VDscp: WMD = −1.34, 95% CI: −1.99 to −0.68, P < 0.0001. VDdcp: WMD = −2.00, 95% CI: −2.95 to −1.04, P < 0.0001. Peripapillary VD: WMD = −1.07, 95% CI: −1.70 to −0.43, P = 0.0010). However, there was no statistically significant difference in total FAZ between them (WMD = −0.00, 95% CI: −0.02–0.01, P = 0.84). In addition, for patients with mild NPDR, OCTA could illustrate prominent changes in VDscp, VDdcp, and total FAZ compared with healthy people (VDscp: WMD = −6.11, 95% CI: −9.90 to −2.32, P = 0.002. VDdcp: WMD = −4.26, 95% CI: −5.95 to −2.57, P < 0.00001. FAZ: WMD = 0.06, 95% CI: 0.01–0.11, P = 0.03).
In diabetic patients with or without retinopathy, the parameters of OCTA such as VDscp, VDdcp, and peripapillary vessel density were demonstrated as potential biomarkers in monitoring the early alterations of retinal microangiopathy, while total FAZ may have no significant changes in diabetic patients without retinopathy.