Existing research on the relationship between body mass index (BMI) and astigmatism yields inconsistent results. This study analyses this association in a nationally representative sample of adolescents.
This retrospective, cross-sectional study included Israeli adolescents who underwent medical assessments before mandatory military service between 2011 and 2022. BMI was categorised based on the US age- and sex-matched percentiles. Astigmatism was categorised by magnitude [low-moderate: 0.75 to <3.00 diopters (D), high: ≥3.00 D], and axis orientation [with-the-rule (WTR), against-the-rule (ATR), or oblique (OBL)]. Sex-stratified regression models adjusted for sociodemographic variables were used.
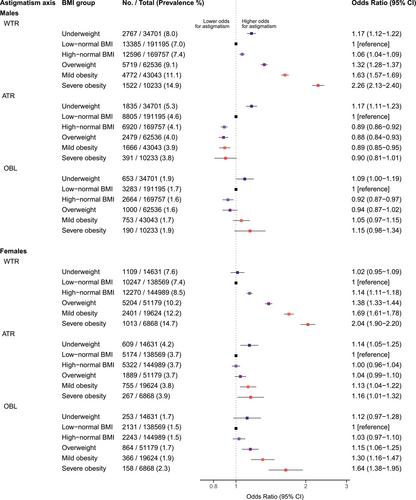
Of 935 989 adolescents evaluated, 887 325 were included [511 465 (57.6%) males, mean age 17.2 years]. Astigmatism was diagnosed in 123 675 (13.9%) adolescents, of whom 117 081 (13.2%) had low-moderate and 6594 (0.7%) had high astigmatism. WTR astigmatism was the most prevalent (8.2%), followed by ATR (4.1%) and OBL (1.6%) types. Compared with low-normal BMI (5th to 50th percentile), the adjusted ORs for total astigmatism increased with increasing BMI, peaking at 1.65 (1.57–1.74) in males and 1.74 (1.64–1.86) in females with severe obesity. ORs were accentuated for high astigmatism, reaching 3.51 (3.01–4.09) in males, and 3.45 (2.83–4.22) in females with severe obesity. WTR astigmatism demonstrated the strongest association with BMI, with ORs reaching 2.26 (2.13–2.40) in males and 2.04 (1.90–2.20) in females with severe obesity. The results persisted in a series of subgroup analyses.
Obesity is associated with higher odds of astigmatism in adolescence. Further investigation into the role of weight management in astigmatism development is warranted.