To explore the value of cell morphology, immunophenotype, and gene alterations of serosal effusion in the diagnosis of lymphoma.
Serosal effusion of 69 cases of lymphoma patients were collected, including 36 cases with malignant effusion and 33 cases with nonmalignant effusion. Ordinary cytology, liquid-based cytology, cellblock, and immunocytochemical staining were performed in each case, some cases were detected by fluorescence in situ hybridization for C-MYC, BCL2, and BCL6 gene translocations. T/B cell ratio in malignant and nonmalignant serosal effusions was analyzed and compared by flow cytometry (FCM) and immunohistochemical (IHC), respectively. The prognostic value of serous effusion in diffuse large B-cell lymphoma (DLBCL) was investigated and another 20 DLBCL cases without effusion were successively selected as control.
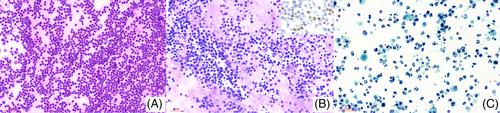
The number of naive lymphocytes, apoptotic bodies, and mitotic figures were more common in malignant effusions compared with nonmalignant effusions (p < .01). The top three lymphomas in malignant effusion were DLBCL (19/36, 52.8%), mantle cell lymphoma (MCL) (4/36, 11.1%, 3 blastoid variant) and high-grade B-cell lymphoma (HGBL) (4/36, 11.1%). T/B cell ratio by FCM analysis ranged from 0.00 to 0.55 (mean 0.084) in malignant effusion, and 2.58 to 984.00 (mean 249.9) in nonmalignant effusion. The difference was significant (p = .017). The T/B cell ratio by IHC analysis ranged from 0.02 to 3.00 (mean 0.200) in malignant effusion, and 2.00–100.00 (mean 34.10) in nonmalignant effusion. The difference was significant (p = .017). In the effusions involving DLBCL, most effusions were present at the time of diagnosis (57.9%); single pleural effusions were more common (36.8%). The median overall survival times of patients with malignant effusion, nonmalignant effusion and DLBCL without serous effusion were 11, 17, and 23 months respectively (p = .04). Three patients of HGBL died, and the overall survival times were 5, 8, and 9 months, respectively.
The cytomorphological characteristics combined with immunophenotype, FCM, gene rearrangement, and other tests can diagnose and classify patients with effusion as the first symptom. The T/B cell ratio is less than 1 by FCM or IHC suggesting a malignant serosal effusion. The presence of malignant effusion in DLBCL patients is an important clue for poor prognosis.