下载PDF
{"title":"TP53 mutations in urothelial carcinoma: not all one and the same†","authors":"Alexis R Barr, Amy Burley, Anna Wilkins","doi":"10.1002/path.6335","DOIUrl":null,"url":null,"abstract":"<p>Systemic therapy options for urothelial carcinoma have expanded in recent years, with both immunotherapy and cytotoxic chemotherapy being widely available. However, we lack biomarkers to select which drug is likely to work best in individual patients. A new article in this journal by Jin, Xu, Su, <i>et al</i> reports that disruptive versus non-disruptive <i>TP53</i> mutations may guide these personalised therapy choices. Intriguingly, patients with disruptive <i>TP53</i> tumour mutations had poor overall survival versus those with non-disruptive <i>TP53</i> mutations or wild type <i>TP53</i> but responded particularly well to immunotherapy. Of relevance, an increased tumour mutational burden and increased effector CD8<sup>+</sup> T-cell infiltration was seen in tumours with disruptive mutations. The impact of different <i>TP53</i> mutations on prognosis and therapy choices appears to be tumour- and therapy-type specific, with no clear consensus on overall tumour phenotype according to type of mutation. Nonetheless, profiling of specific types of <i>TP53</i> mutation is increasingly clinically feasible with targeted sequencing or immunohistochemistry. There is an urgent need for additional studies in urothelial cancer clarifying how the type of <i>TP53</i> mutation present within a tumour can best be used as a predictive biomarker. Further important remaining questions include the impact of <i>TP53</i> mutations on other clinically important aspects of the tumour microenvironment, including cancer-associated fibroblasts. Furthermore, the impact of gain-of-function mutations in <i>TP53</i> and other related genes signalling upstream or downstream of <i>TP53</i> is of wide interest. © 2024 The Author(s). <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"264 2","pages":"125-128"},"PeriodicalIF":5.6000,"publicationDate":"2024-07-24","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6335","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6335","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
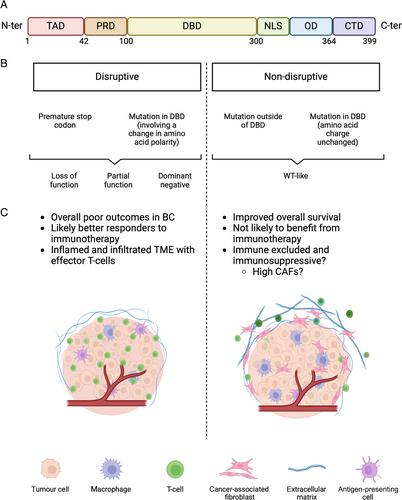
Systemic therapy options for urothelial carcinoma have expanded in recent years, with both immunotherapy and cytotoxic chemotherapy being widely available. However, we lack biomarkers to select which drug is likely to work best in individual patients. A new article in this journal by Jin, Xu, Su, et al reports that disruptive versus non-disruptive TP53 mutations may guide these personalised therapy choices. Intriguingly, patients with disruptive TP53 tumour mutations had poor overall survival versus those with non-disruptive TP53 mutations or wild type TP53 but responded particularly well to immunotherapy. Of relevance, an increased tumour mutational burden and increased effector CD8+ T-cell infiltration was seen in tumours with disruptive mutations. The impact of different TP53 mutations on prognosis and therapy choices appears to be tumour- and therapy-type specific, with no clear consensus on overall tumour phenotype according to type of mutation. Nonetheless, profiling of specific types of TP53 mutation is increasingly clinically feasible with targeted sequencing or immunohistochemistry. There is an urgent need for additional studies in urothelial cancer clarifying how the type of TP53 mutation present within a tumour can best be used as a predictive biomarker. Further important remaining questions include the impact of TP53 mutations on other clinically important aspects of the tumour microenvironment, including cancer-associated fibroblasts. Furthermore, the impact of gain-of-function mutations in TP53 and other related genes signalling upstream or downstream of TP53 is of wide interest. © 2024 The Author(s). The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
尿路上皮癌中的 TP53 基因突变:不尽相同†。
近年来,尿路上皮癌的全身治疗方案不断扩大,免疫疗法和细胞毒性化疗都已广泛应用。然而,我们缺乏生物标志物来选择哪种药物对患者的疗效最好。金、徐、苏等人在本刊上发表的一篇新文章指出,TP53突变的破坏性与非破坏性可指导这些个性化疗法的选择。耐人寻味的是,与非破坏性TP53突变或野生型TP53相比,破坏性TP53肿瘤突变患者的总生存率较低,但对免疫疗法的反应特别好。与此相关的是,在具有破坏性突变的肿瘤中,肿瘤突变负荷增加,效应CD8+ T细胞浸润增加。不同的TP53突变对预后和治疗选择的影响似乎与肿瘤和治疗类型有关,对于突变类型导致的整体肿瘤表型还没有明确的共识。尽管如此,利用靶向测序或免疫组化技术分析特定类型的 TP53 突变在临床上越来越可行。目前迫切需要对尿路癌进行更多的研究,以明确如何最好地将肿瘤中出现的 TP53 突变类型用作预测性生物标记物。其他尚存的重要问题包括 TP53 突变对肿瘤微环境(包括癌症相关成纤维细胞)的其他临床重要方面的影响。此外,TP53和TP53上游或下游信号传递的其他相关基因的功能增益突变的影响也引起了广泛关注。© 2024 作者。病理学杂志》由 John Wiley & Sons Ltd 代表大不列颠及爱尔兰病理学会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。