Most human infections with non-typhoid Salmonella (NTS) or Campylobacter are zoonotic in nature and acquired though consumption of contaminated food of mainly animal origin. However, individuals may also acquire salmonellosis or campylobacteriosis through non-foodborne transmission pathways, such as those mediated by the environment. This emphasizes the need to consider both direct and indirect exposure to livestock sources as a possible transmission route for NTS and Campylobacter. Therefore, this study aimed at assessing whether salmonellosis and campylobacteriosis incidence is spatially associated with exposure to livestock (i.e. small ruminants, dairy cows, veal calves, laying hens, broiler chickens and pigs) in the Netherlands for the years 2007–2019 and 2014–2019 respectively.
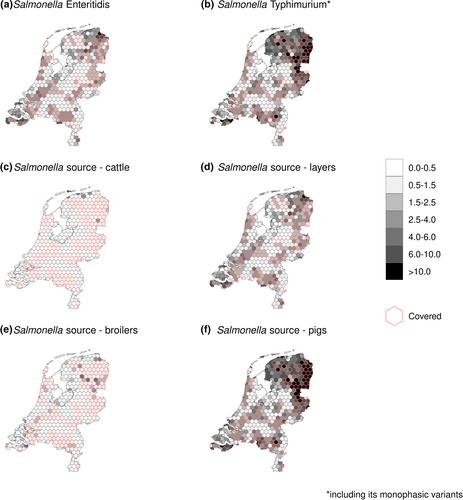
Risk factors (population-weighted number of animals) and their population attributable fractions were determined using a Poisson regression model with a log-link function fitted using integrated nested Laplace approximation. The analyses were performed for different hexagonal sizes (90, 50, 25 and 10 km2) and accounted for geographical coverage of the diagnostic laboratory catchment areas. Moreover, serological data were used to look into the possible effects of acquired immunity due to repeated exposure to the pathogen through the environment that would potentially hinder the analyses based on the incidence of reported cases. A linear mixed-effects model was then fitted where the postal code areas were included as a random effect. Livestock was not consistently significantly associated with acquiring salmonellosis or campylobacteriosis in the Netherlands.
Results showed that living in livestock-rich areas in the Netherlands is not a consistently significant, spatially restricted risk factor for acquiring salmonellosis or campylobacteriosis, thereby supporting current knowledge that human infections with Salmonella and Campylobacter are mainly foodborne.