Pan-cancer evaluation of tumor-infiltrating lymphocytes and programmed cell death protein ligand-1 in metastatic biopsies and matched primary tumors
Zakhia El Beaino, Célia Dupain, Grégoire Marret, Xavier Paoletti, Laëtitia Fuhrmann, Charlotte Martinat, Yves Allory, Maral Halladjian, Ivan Bièche, Christophe Le Tourneau, Maud Kamal, Anne Vincent-Salomon
下载PDF
{"title":"Pan-cancer evaluation of tumor-infiltrating lymphocytes and programmed cell death protein ligand-1 in metastatic biopsies and matched primary tumors","authors":"Zakhia El Beaino, Célia Dupain, Grégoire Marret, Xavier Paoletti, Laëtitia Fuhrmann, Charlotte Martinat, Yves Allory, Maral Halladjian, Ivan Bièche, Christophe Le Tourneau, Maud Kamal, Anne Vincent-Salomon","doi":"10.1002/path.6334","DOIUrl":null,"url":null,"abstract":"<p>Tumor immunological characterization includes evaluation of tumor-infiltrating lymphocytes (TILs) and programmed cell death protein ligand-1 (PD-L1) expression. This study investigated TIL distribution, its prognostic value, and PD-L1 expression in metastatic and matched primary tumors (PTs). Specimens from 550 pan-cancer patients of the SHIVA01 trial (NCT01771458) with available metastatic biopsy and 111 matched PTs were evaluated for TILs and PD-L1. Combined positive score (CPS), tumor proportion score (TPS), and immune cell (IC) score were determined. TILs and PD-L1 were assessed according to PT organ of origin, histological subtype, and metastatic biopsy site. We found that TIL distribution in metastases did not vary according to PT organ of origin, histological subtype, or metastatic biopsy site, with a median of 10% (range: 0–70). TILs were decreased in metastases compared to PT (20% [5–60] versus 10% [0–40], <i>p</i> < 0.0001). CPS varied according to histological subtype (<i>p</i> = 0.02) and biopsy site (<i>p</i> < 0.02). TPS varied according to PT organ of origin (<i>p</i> = 0.003), histological subtype (<i>p</i> = 0.0004), and metastatic biopsy site (<i>p</i> = 0.00004). TPS was higher in metastases than in PT (<i>p</i> < 0.0001). TILs in metastases did not correlate with overall survival. In conclusion, metastases harbored fewer TILs than matched PT, regardless of PT organ of origin, histological subtype, and metastatic biopsy site. PD-L1 expression increased with disease progression. © 2024 The Author(s). <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"264 2","pages":"186-196"},"PeriodicalIF":5.2000,"publicationDate":"2024-07-29","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6334","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://pathsocjournals.onlinelibrary.wiley.com/doi/10.1002/path.6334","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
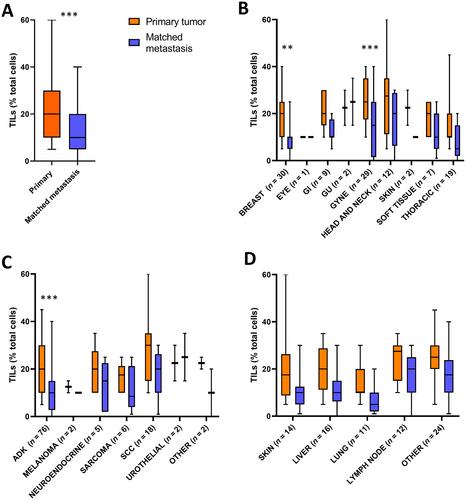
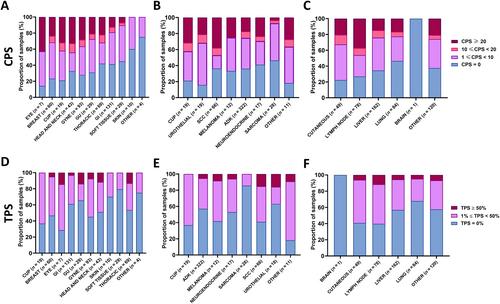
Tumor immunological characterization includes evaluation of tumor-infiltrating lymphocytes (TILs) and programmed cell death protein ligand-1 (PD-L1) expression. This study investigated TIL distribution, its prognostic value, and PD-L1 expression in metastatic and matched primary tumors (PTs). Specimens from 550 pan-cancer patients of the SHIVA01 trial (NCT01771458) with available metastatic biopsy and 111 matched PTs were evaluated for TILs and PD-L1. Combined positive score (CPS), tumor proportion score (TPS), and immune cell (IC) score were determined. TILs and PD-L1 were assessed according to PT organ of origin, histological subtype, and metastatic biopsy site. We found that TIL distribution in metastases did not vary according to PT organ of origin, histological subtype, or metastatic biopsy site, with a median of 10% (range: 0–70). TILs were decreased in metastases compared to PT (20% [5–60] versus 10% [0–40], p < 0.0001). CPS varied according to histological subtype (p = 0.02) and biopsy site (p < 0.02). TPS varied according to PT organ of origin (p = 0.003), histological subtype (p = 0.0004), and metastatic biopsy site (p = 0.00004). TPS was higher in metastases than in PT (p < 0.0001). TILs in metastases did not correlate with overall survival. In conclusion, metastases harbored fewer TILs than matched PT, regardless of PT organ of origin, histological subtype, and metastatic biopsy site. PD-L1 expression increased with disease progression. © 2024 The Author(s). The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
对转移性活检组织和匹配的原发肿瘤中的肿瘤浸润淋巴细胞和程序性细胞死亡蛋白配体-1进行泛癌评估。
肿瘤免疫学特征描述包括对肿瘤浸润淋巴细胞(TIL)和程序性细胞死亡蛋白配体-1(PD-L1)表达的评估。本研究调查了转移性肿瘤和匹配的原发性肿瘤(PT)中的TIL分布、其预后价值和PD-L1表达。研究人员对SHIVA01试验(NCT01771458)中550例泛癌患者的转移性活检标本和111例匹配的原发肿瘤标本进行了TIL和PD-L1评估。确定了综合阳性评分(CPS)、肿瘤比例评分(TPS)和免疫细胞评分(IC)。TIL和PD-L1根据PT的来源器官、组织学亚型和转移活检部位进行评估。我们发现,TIL在转移灶中的分布并不因PT来源器官、组织学亚型或转移活检部位而异,中位数为10%(范围:0-70)。与 PT 相比,转移灶中的 TIL 数量减少(20% [5-60] 对 10% [0-40],p
本文章由计算机程序翻译,如有差异,请以英文原文为准。