This scoping review assesses existing research on observation units, examining diagnoses, clinical outcomes, finances, and health system comparisons to identify knowledge gaps related to patients in dedicated emergency observation units.
The scoping review follows the Joanna Briggs Institute (JBI) methodology and was published prior to the review on Open Science Framework. Databases searched included MEDLINE/PubMed, Embase (Ovid), and CINAHL (Ebsco), with unpublished studies and gray literature identified via Web of Science. Articles were screened and extracted by two reviewers in Covidence. Any data or inclusion criteria inconsistencies were resolved through arbitration by a third researcher or by team consensus. Data were transferred to Excel for analysis.
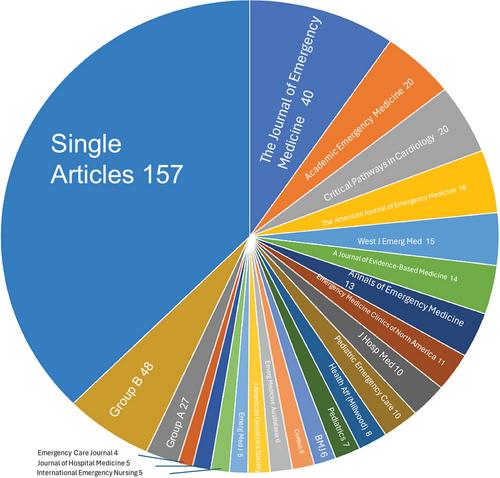
A total of 1061 studies were assessed for eligibility: 461 articles met study inclusion criteria and 433 were excluded for being abstracts only. Of these 461 articles, the majority focused on cardiac diagnoses (111/461, 24%) and adult populations (321/461, 70%) and are retrospective or cohort studies (241/461, 52%). Fifty-four articles (12%) belonged to expert opinion category. Length of stay (191/461, 41%) is the most common outcome measure followed by morbidity/mortality (189/461, 41%), admission/failure rate (169/461, 37%), and protocol assessments (120/461, 26%). Few articles focused on staff models and structure but 121 of 461 (26%) mentioned it. Note that 162 (35%) measured hospital finances, and 120 (26%) articles performed some direct comparison to other forms of observation.
While reimbursement and cardiac conditions are frequently assessed in emergency department observation unit literature, there is paucity of discussion on staffing models and other diagnoses remain less frequently explored. This review aims to spotlight future research areas in observation medicine.