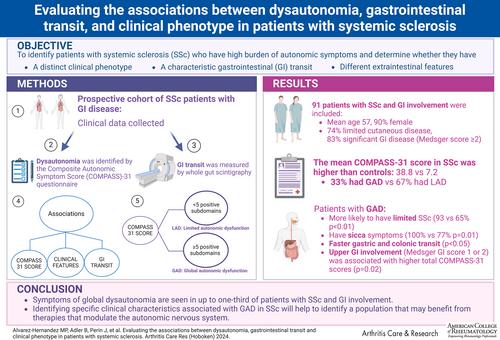
Our objective was to identify patients with systemic sclerosis (SSc) with a high burden of autonomic symptoms and to determine whether they have a distinct clinical phenotype, gastrointestinal (GI) transit, or extraintestinal features.
In a prospective cohort of patients with SSc with GI disease, clinical data were systematically obtained at routine visits. Dysautonomia was identified by the Composite Autonomic Symptom Score (COMPASS)-31questionnaire. GI transit was measured by whole-gut scintigraphy. Associations between total COMPASS-31 scores and clinical features, GI symptoms, and transit were evaluated. Comparisons between patients with global autonomic dysfunction (GAD; ≥5 positive COMPASS-31 subdomains) and those with limited autonomic dysfunction (LAD; <5 positive subdomains) were also studied.
A total of 91 patients with SSc and GI involvement were included (mean age 57 years, 90% female, 74% limited cutaneous disease, 83% significant GI disease [Medsger score ≥2]). The mean COMPASS-31 score in patients with SSc was higher than controls (38.8 vs 7.2); 33% had GAD, and 67% had LAD. Patients with GAD were more likely to have limited SSc (93% vs 65%; P < 0.01) and have sicca symptoms (100% vs 77%; P = 0.01). Gastric and colonic transit were faster in patients with GAD (P < 0.05). Upper GI involvement (Medsger GI score of 1 or 2) was associated with higher total COMPASS-31 scores (P = 0.02).
Symptoms of global dysautonomia are seen in up to one-third of patients with SSc and GI involvement. Identifying specific clinical characteristics associated with GAD in SSc will help to identify a population that may benefit from therapies that modulate the autonomic nervous system.