Mild cognitive impairment (MCI) is a significant public health concern and a potential precursor to Alzheimer's disease (AD). This study leverages electronic health record (EHR) data to explore rural-urban differences in MCI incidence, risk factors, and healthcare navigation in West Michigan.
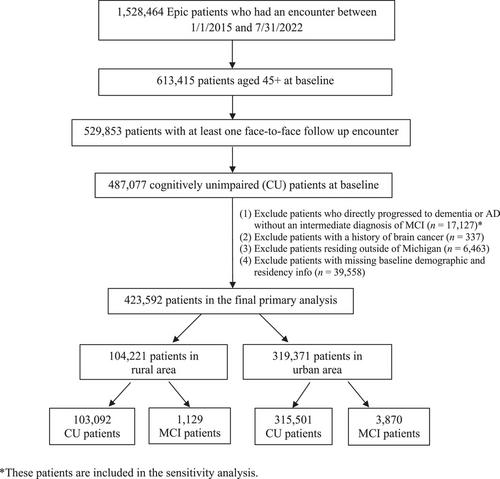
Analysis was conducted on 1,528,464 patients from Corewell Health West, using face-to-face encounters between 1/1/2015 and 7/31/2022. MCI cases were identified using International Classification of Diseases (ICD) codes, focusing on patients aged 45+ without prior MCI, dementia, or AD diagnoses. Incidence rates, cumulative incidences, primary care physicians (PCPs), and neuropsychology referral outcomes were examined across rural and urban areas. Risk factors were evaluated through univariate and multivariate Cox regression analyses. The geographic distribution of patient counts, hospital locations, and neurology department referrals were examined.
Among 423,592 patients, a higher MCI incidence rate was observed in urban settings compared to rural settings (3.83 vs. 3.22 per 1,000 person-years). However, sensitivity analysis revealed higher incidence rates in rural areas when including patients who progressed directly to dementia. Urban patients demonstrated higher rates of referrals to and completion of neurological services. While the risk factors for MCI were largely similar across urban and rural populations, urban-specific factors for incident MCI are hearing loss, inflammatory bowel disease, obstructive sleep apnea, insomnia, being African American, and being underweight. Common risk factors include diabetes, intracranial injury, cerebrovascular disease, coronary artery disease, stroke, Parkinson's disease, epilepsy, chronic obstructive pulmonary disease, depression, and increased age. Lower risk was associated with being female, having a higher body mass index, and having a higher diastolic blood pressure.
This study highlights rural-urban differences in MCI incidence and access to care, suggesting potential underdiagnosis in rural areas likely due to reduced access to specialists. Future research should explore socioeconomic, environmental, and lifestyle determinants of MCI to refine prevention and management strategies across geographic settings.