To explore the efficacy of a prediction model based on diffusion-weighted imaging (DWI) features extracted from deep learning (DL) and radiomics combined with clinical parameters and apparent diffusion coefficient (ADC) values to identify microsatellite instability (MSI) in endometrial cancer (EC).
This study included a cohort of 116 patients with EC, who were subsequently divided into training (n = 81) and test (n = 35) sets. From DWI, conventional radiomics features and convolutional neural network-based DL features were extracted. Random forest (RF) and logistic regression were adopted as classifiers. DL features, radiomics features, clinical variables, ADC values, and their combinations were applied to establish DL, radiomics, clinical, ADC, and combined models, respectively. The predictive performance was evaluated through the area under the receiver operating characteristic curve (AUC), total integrated discrimination index (IDI), net reclassification index (NRI), calibration curves, and decision curve analysis (DCA).
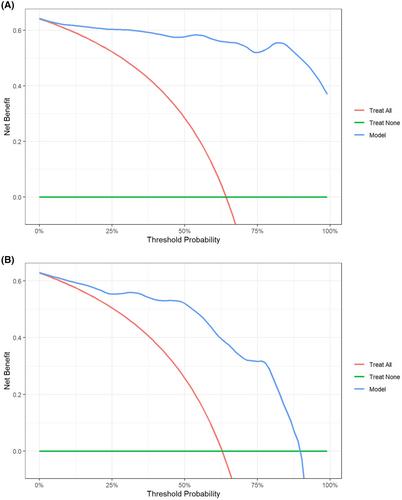
The optimal predictive model, based on an RF classifier, comprised four DL features, three radiomics features, two clinical variables, and an ADC value. In the training and test sets, this model exhibited AUC values of 0.989 (95% CI: 0.935–1.000) and 0.885 (95% CI: 0.731–0.967), respectively, demonstrating different degrees of improvement compared with the clinical, DL, radiomics, and ADC models (AUC-training = 0.671, 0.873, 0.833, and 0.814, AUC-test = 0.685, 0.783, 0.708, and 0.713, respectively). The NRI and IDI analyses revealed that the combined model resulted in improved risk reclassification of the MSI status compared to the clinical, radiomics, DL, and ADC models. The calibration curves and DCA indicated good consistency and clinical utility of this model, respectively.
The predictive model based on DWI features extracted from DL and radiomics combined with clinical parameters and ADC values could effectively assess the MSI status in EC.