With advancements in respiratory interventional techniques, bronchoscopic intervention technology has emerged as a viable approach for managing postintubation tracheal stenosis (PITS). However, there was a paucity of research investigating the potential impact of stenosis characteristics and morphology (such as stenosis degree, length, type, and morphology) on bronchoscopic intervention treatment prognosis for PITS patients. This study was to assess the impact of various preoperative stenosis characteristic factors on the bronchoscopic cure rate among patients.
This is a retrospective study analyzing the medical records of patients with PITS who received bronchoscopic intervention at the tertiary interventional pulmonology center.
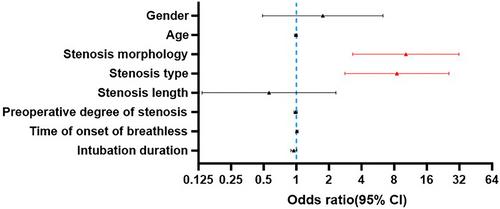
Among the cases, 115 individuals achieved a in a success rate of 79.86% for bronchoscopic intervention therapy and were assigned to Group S. On the other hand, 29 cases required surgical intervention, accounting for a surgical treatment rate of 20.14% and were assigned to Group F. The stenosis in the Group F predominantly exhibited irregular shapes with scar granulation accompanied by tracheal chondromalacia collapse. Patients in group S experienced fewer total procedures, rigid bronchoscopy treatment, intraoperative hypoxemia, needed emergency re-bronchoscopy in 24 h and transferred to ICU postoperatively. Patients with pure scar and granuloma, the rate of bronchoscopic success cure was higher than patients with scar granulation accompanied by tracheal chondromalacia (odds ratio: 8.208; 95% confidence interval: 2.755–24.459), and regular stenosis morphology was associated with a higher bronchoscopic success cure rate (odds ratio: 9.463; 95% confidence interval: 3.128–28.623).
Irregular airway stenosis, chondromalacia or airway collapse are key factors affecting the success rate of bronchoscopic treatment for post-intubation tracheal stenosis.
Level of evidence: 4 (historically controlled studies).