Focal laser ablation (FLA) serves as a targeted therapy for prostate cancer (PCa). Clinical studies have demonstrated significant variations in ablation volumes with consistent fiber configurations. Consequently, a prediction model is needed for the safe application of FLA in treating PCa.
This study aimed to evaluate the reproducibility of FLA–induced temperature profiles in controlled ex vivo experiments using clinical laser treatment protocols. Additionally, it sought to examine the effectiveness of the CEM43 model in predicting the zone of irreversible damage (ZID) and to compare these findings with outcomes derived from the Arrhenius model.
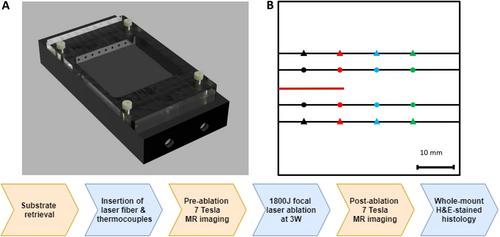
Freshly excised postmortem human prostate and porcine liver specimens were used for controlled ex vivo ablation. Tissues were secured in a Perspex sample holder for precise placement of the laser fiber and thermocouples. FLA was conducted with a 1064-nm Nd:YAG laser at 3 W in continuous-wave mode for 10 min. Pre– and post–FLA 3D T1-weighted 7 T MRI scans were obtained to assess the treatment area. Whole-mount hematoxylin and eosin histological slides were prepared and digitized. On histology, the ZID was defined as the total of vaporized, carbonized, and coagulated tissue. A 2D thermal development map was created from temperature data, using bi-cubic interpolation. The cumulative equivalent thermal isoeffect dose at 43°C in minutes (CEM43) model was applied to predict the ZID, with 240 equivalent minutes (240-CEM43) used as the damage threshold. Additionally, the Arrhenius thermal model was used for comparison of CEM43 results. Predicted ZIDs were compared to MRI and histology.
FLA treatment was performed on ex vivo human prostate samples (n = 2) and porcine liver specimens (n = 5). For human prostate tissue, FLA did not result in an identifiable ZID upon histological macroscopic examination or a lesion on MRI. Ex vivo porcine liver samples showed a clearly demarcated oval-shaped hyperintense lesion surrounding the laser fiber tip on post–FLA MRI. The MRI lesion (range 1.6–2.1 cm2) corresponded with the shape and location of the ZID on histology, but was smaller (median 1.7 vs. 3.2, p = 0.02). Histological examination of porcine liver samples revealed ZIDs ranging from 2.1 to 4.1 cm2, whereas 240-CEM43–predicted ZIDs ranged from 3.3 to 3.8 cm2. Although the median 240-CEM43–predicted ZID was not significantly larger than the histology ZID (3.8 vs. 3.2 cm2, p = 0.22), it tended to overpredict the histological results in most experiments. The median Arrhenius-predicted ZID was similar to the histological ZID (3.2 vs. 3.2 cm2, p = 0.56), but varied in size when comparing individual experiments (range 2.5–3.2 cm2).
FLA on ex vivo human prostate showed no thermal damage on histopathology or MRI. Ex vivo porcine liver FLA resulted in identifiable ZID on histology and lesions on MRI. 240-CEM43 generally overestimated the ZID and had less variability compared to histology. Results from the Arrhenius model were in better agreement with the histology findings, but still did not predict the individual FLA–induced histological thermal damage. Inter-experiment ZID variability underlines the need for developing a more comprehensive predictive dosimetry model for FLA in PCa treatment.