In addition to the oscillatory brain activity, the nonoscillatory (scale-free) components of the background electroencephalogram (EEG) may provide further information about the complexity of the underlying neuronal network. As epilepsy is considered a network disease, such scale-free metrics might help to delineate the epileptic network. Here, we performed an analysis of the sleep oscillatory (spindle, slow wave, and rhythmic spectral power) and nonoscillatory (H exponent) intracranial EEG using multiple interictal features to estimate whether and how they deviate from normalcy in 38 adults with drug-resistant epilepsy.
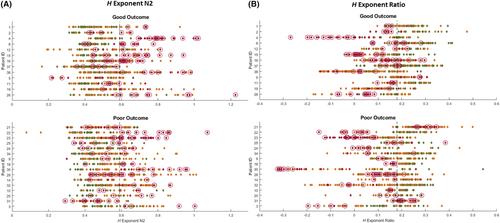
To quantify intracranial EEG abnormalities within and outside the seizure onset areas, patients' values were adjusted based on normative maps derived from the open-access Montreal Neurological Institute open iEEG Atlas. In a subset of 29 patients who underwent resective surgery, we estimated the predictive value of these features to identify the epileptogenic zone in those with a good postsurgical outcome.
We found that distinct sleep oscillatory and nonoscillatory metrics behave differently across the epileptic network, with the strongest differences observed for (1) a reduction in spindle activity (spindle rates and rhythmic sigma power in the 10–16 Hz band), (2) a higher rhythmic gamma power (30–80 Hz), and (3) a higher H exponent (steeper 1/f slope). As expected, epileptic spikes were also highest in the seizure onset areas. Furthermore, in surgical patients, the H exponent achieved the highest performance (balanced accuracy of .76) for classifying resected versus nonresected channels in good outcome patients.
This work suggests that nonoscillatory components of the intracranial EEG signal could serve as promising interictal sleep candidates of epileptogenicity in patients with drug-resistant epilepsy. Our findings further advance the understanding of epilepsy as a disease, whereby absence or loss of sleep physiology may provide information complementary to pathological epileptic processes.