Pregnancy involves changes in maternal metabolism that differ between normal-weight women and women with overweight or obesity, including changes in glucose, insulin, lipids, and adipokines. These changes contribute to altered risk profiles for adverse outcomes for both mother and child during pregnancy, childbirth, and postpartum. We explored associations between visceral fat and prepregnancy body mass index (pBMI), respectively, with glucose and lipid metabolism, as well as with adipokines and C-reactive protein (CRP), measured fasting in early and late pregnancy. We hypothesized that among women with pBMI ≥35 kg/m2, visceral fat measured around gestational week 18 (visceral fat18) would show associations with greater number of metabolic variables during pregnancy, than pBMI.
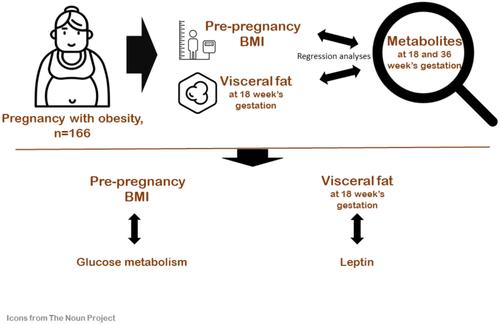
This prospective longitudinal cohort study was conducted at the Department of Gynecology and Obstetrics at Drammen Hospital from 2016 to 2019. We included 166 nulliparous (47.6%) and parous pregnant women with pBMI ≥35 kg/m2 and singleton pregnancy. Women with type 1 diabetes were excluded. We evaluated associations of pBMI and visceral fat estimated with bioimpedance weight around gestational week 18 (visceral fat18) with fasting metabolic measures around gestational weeks 18 and 36 using median regression models. We used the paired t-test or the Wilcoxon signed-rank test, as appropriate, to analyze changes in metabolic measures from early to late pregnancy, and median regression to estimate crude and adjusted differences in medians of 21 maternal metabolic measures associated with one-unit changes in pBMI and visceral fat18, respectively.
pBMI and visceral fat18 were highly correlated and showed associations with similar metabolic measures in pregnancy in crude analysis. After mutual adjustment for each other in addition to age and parity, pBMI was associated with glucose metabolism, in particular fasting insulin, whereas visceral fat18 was primarily associated with leptin.
Among pregnant women with BMI ≥35 kg/m2, easily obtainable pBMI and the more resource-demanding estimate of visceral fat18 exhibit divergent associations with metabolic measures; pBMI was positively associated with insulin, glucose, and HbA1c, while visceral fat18 was positively associated with leptin. We did not find visceral fat18 to be associated with greater number of metabolic factors than pBMI.