Full blood examinations, often referred to as FBE, are commonly ordered postoperatively, despite limited utility in many of its markers in the acute phase. It is estimated that in the 2022–2023 financial year, the Australian healthcare system billed over $13 million for full blood examinations (FBEs) to Medicare. This study aims to assess the cost of using FBE following surgery. We explore potential cost savings by using a haemoglobin examination (HE) in replace of FBE, with both tests run on identical machines, producing the same result, but at a fraction of the cost.
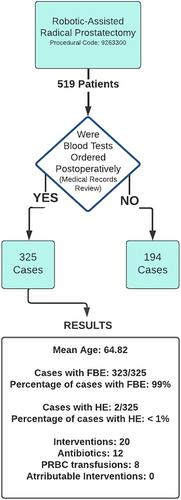
A retrospective analysis was conducted at a single institution, including all patients who underwent minimally invasive laparoscopic pelvic surgeries between 1/7/2017 and 30/6/2019. Patient records were examined to identify patient demographics, postoperative pathology tests and interventions. Patients who received FBE in the first 24 h following surgery were identified and included in the study. Using national surgery and admission statistics, a potential cost-saving analysis will be performed.
Among 519 men who underwent robotic-assisted pelvic surgery, 325 patients had routine postoperative investigations, with 323 receiving FBE and 2 receiving HE. Abnormal results were found in the majority of patients that underwent FBE. Eight patients received packed red blood cell transfusion, none of these meeting the hospital-specific criteria for transfusion protocol. Twelve patients received antibiotics, none were in response to abnormal FBE, with all patients experiencing a fever, given prophylactically or in the days following the surgery. FBE and HE are both listed on the Medicare Benefits Scheme at $16.95 and $7.85, respectively, the difference being $9.10. Extrapolating the existing data, within the first 24 h following surgery, the estimated savings were $8818, with savings increasing accumulatively with longer observation intervals following surgery. When similar savings are applied to national figures, the potential savings to the Australian Public Healthcare system likely exceeds millions.
Our study revealed that over half of the patients who underwent a RARP received FBE within the first 24 h postoperatively, the vast majority of which exhibited abnormal results that were not acted upon. These findings substantiate the limited utility of FBE in the postoperative setting. Cell markers observed in FBE are predominantly subjective, but consensus exists regarding the importance of evaluating haemoglobin levels postoperatively. Considering that one in four hospital admissions involves surgical procedures, and a $9.10 price differential between FBE and HE, the potential annual economic impact of utilising routine FBEs for assessing haemoglobin levels immediately after surgery is likely to reach millions. Although having obvious flaws, these results underscore the potential accumulative cost arising from everyday clinical judgement and the importance of thoughtful consideration when ordering pathology.
The routine ordering of FBE postoperatively, without properly considering its indication, incurs significant costs. This study highlights the potential cost savings by HE instead, emphasising the need for revaluation and appropriate utilisation of pathology tests in the immediate postoperative period given the physiological acute phase response expected postoperatively.