Recently, antibiotics use in uncomplicated acute diverticulitis (AD) has been controversial in Europe. The American Gastroenterological Association (AGA) in their 2015 guidelines recommend their selective use. Our study highlights their role in outpatient management.
We queried the Diamond Network through TriNetX-Research Network including 92 healthcare organizations. We included large intestine diverticulitis without perforation, abscess or bleeding. Exclusion criteria included any of sepsis criteria, CRP > 15 mg/L, immunodeficiency or HIV, coronary artery disease, chronic kidney disease, history of Crohn's disease or ulcerative colitis, heart failure, hypertension, diabetes or any of the following in the 3 months before study date; clostridium difficile (C. diff) infection, diverticulitis or antibiotics. Patients with AD were divided into two cohorts; patients on antibiotics, and patients not on antibiotics. Cohorts were compared after propensity-score matching (PSM).
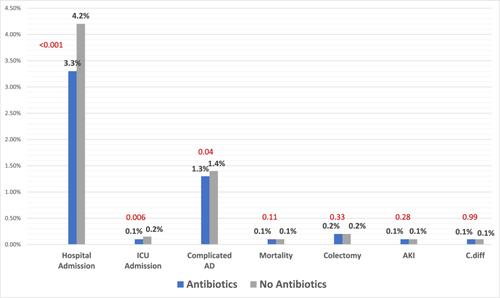
214,277 patients met inclusion criteria. 58.9% received antibiotics, and 41% did not. After PSM, both cohorts had 84,320. Rate of hospital admission was lower in the antibiotic group (3.3% vs 4.2%, p < .001). There was a statistical difference between ICU admission (0.1% vs 0.15%, p < .01) and the rate of bowel perforation, peritonitis, abscess formation or bleeding (1.3% vs 1.4%, p = .044). There was no difference in mortality (0.1% vs 0.1%, p = .11), C. diff (0.1% vs 0.1%, p = .9), colectomies (0.2% vs 0.2%, p = .33), or Acute Kidney Injury (AKI) (0.1% vs 0.1%, p = .28).
Outpatient use of antibiotics in patients with uncomplicated AD is associated with lower rates of hospital admissions and complications without changing mortality rate or surgical intervention.