In the last decade, the Netherlands has implemented various diagnostic and treatment strategies to enhance rectal cancer outcomes. This study, using data from the Prospective Dutch ColoRectal Cancer (PLCRC) cohort, investigates whether these multidisciplinary advancements have translated into improved health-related quality of life (HRQoL) and functional outcomes for the general Dutch rectal cancer population.
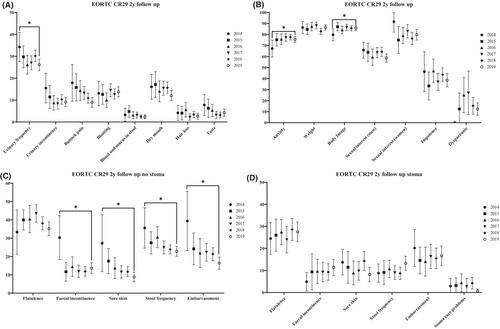
Patients with Stage I–III rectal cancer enrolled in the PLCRC cohort were included. HRQoL and functional outcomes were assessed 1 and 2 years after diagnosis using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30), EORTC QLQ Colorectal Cancer 29 and the Low Anterior Resection Syndrome score. HRQoL and functional outcomes were compared based on year of diagnosis (2014–2019).
A total of 1294 patients were included. Two years after diagnosis, patients diagnosed in 2019 (n = 392) had a clinically relevant higher score on physical (8.2, 95% CI 4.1–12.3), role (13.5, 95% CI 7.3–19.7) and social functioning (5.8, 95% CI 0.3–11.2) compared to those diagnosed in 2014 (n = 65). Additionally, patients diagnosed in 2019 experienced less fatigue 2 years after diagnosis compared to those diagnosed in 2014 (−8.6, 95% CI −14.1 to −3.0). The Low Anterior Resection Syndrome score showed no differences.
The findings of this study suggest that over the past decade rectal cancer patients in the Netherlands have witnessed improvements in HRQoL across various domains. Most probably, the improvement is due to a combination of implementation of population screening, a more restrictive neoadjuvant radiotherapy policy and advances in minimally invasive surgery and organ preserving treatment options.