Although perinatal death rates in the Nordic countries are among the lowest in the world, the risk of perinatal death is unevenly distributed across the Nordic countries, despite similarity in health care systems and pregnancy care. Birth registration practices across countries may explain some of the differences. We investigated differences in national registration of perinatal mortality within the Nordic countries and its impact on perinatal mortality according to gestational age.
Each country provided information by answering a questionnaire about registration of perinatal deaths. Furthermore, we collected aggregated count data based on Medical Birth Registries (MBR) from all Nordic countries in 2000 to 2021. Perinatal mortality was defined as stillbirth or neonatal death occurring within first 7 days of life. Data were grouped into six groups by gestational age (GA): extremely preterm (>28 + 0 weeks, subdivided into 22 + 0–23 + 6 and 24 + 0–27 + 6), very preterm (GA 28 + 0–31 + 6), moderate preterm (GA 32 + 0–33 + 6), late preterm (GA 34 + 0–36 + 6), term (GA 37 + 0–40 + 6) and late term or post-term birth (GA ≥ 41 + 0). Perinatal mortality rate and risk ratio with 95% confidence intervals were calculated per country for each gestational age group. For Denmark, separate analyses included and excluded induced abortions.
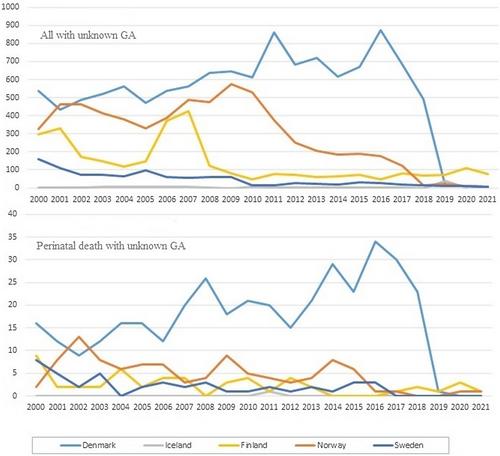
The study included 6 343 805 live births, 22 727 stillbirths and 8932 liveborn infants who died within the first week of life after GA 22 + 0. Further 25 057 births were included with GA < 22 + 0, unknown GA and as a result of induced abortion. Overall, perinatal mortality rates decreased during year 2000–2021 in all Nordic countries. After exclusion of induced abortions, the perinatal mortality rate was similar in the five Nordic countries. The perinatal mortality rate for extremely preterm born infants was highest in Denmark, whereas the highest rate among infants born late term/post-term was in Sweden.
The perinatal mortality rate in the Nordic countries is still decreasing, especially in the group of extremely preterm born infants. This study supports the need for further standardization of birth registration practices to ensure the validity of international comparisons.