NLRP3 inflammasome-related inflammation might play an important role in the pathophysiology of severe CVT. The use of steroids as anti-inflammatory agents in improving severe CVT prognosis remains controversial.
A total of 94 male Sprague–Dawley rats were used. We evaluated the dynamic and association between NLRP3 inflammasome in brain, blood, and CSF and severity in severe CVT rats and/or patients. We also explored the effect of steroids on NLRP3 activation, neurological injury, and CSF circulation disturbance after CVT in animals and/or patients.
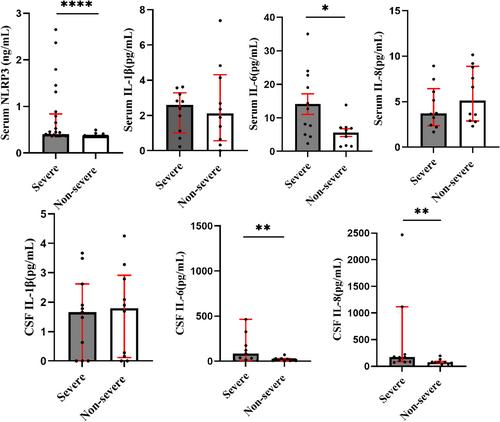
In rats, compared with the sham group, NLRP3-related factors rose on day 1, peaked on day 2 (NLRP3, Sham: 0.79 ± 0.22; day 2: 1.25 ± 0.08, p < 0.01; pro-Caspase-1, Sham: 0.58 ± 0.13, day 2: 1.20 ± 0.44, p < 0.05; GSDMD, Sham: 0.94 ± 0.22, day 2: 1.72 ± 0.46, p < 0.05; pro-IL-1β, Sham: 0.74 ± 0.15, day 2: 1.35 ± 0.09, p < 0.01), decreased on day 7 in rats (n = 4 per group). Thrombus (Sham: 0.00 ± 0.00, day 2: 3.44 ± 0.70, p < 0.0001), infarct size (Sham: 0.00 ± 0.00, day 2: 11.99 ± 6.26, p < 0.01) and neurological deficits appeared similar trend. In 50 patients, serum NLRP3 and IL-6 levels correlated positively with NIHSS (r = 0.4273, p = 0.0020; r = 0.4938, p = 0.0029) and mRS (r = 0.5349, p = 0.0125; r = 0.6213, p = 0.026), while CSF IL-6 correlated positively with mRS on admission (r = 0.5349, p = 0.0125). Compared with baseline, NLRP3 (0.36 (0.36, 0.36) vs. 0.41 (0.37, 0.84), p < 0.0001) and IL-6 decreased (4.06 ± 1.48 vs. 12.03 ± 7.80, p < 0.05), accompanying by improvement of neurological deficits and CSF circulation (all p < 0.01) after steroids therapy in severe CVT patients at discharge and 3 months follow-up. No significant steroid-related adverse effects were observed.
Short-term steroid therapy may improve prognosis of severe CVT by suppressing NLRP3 inflammasome-related inflammation.