In accordance with European Society of Parenteral and Enteral Nutrition guidelines, the combination of malnutrition universal screening tool (MUST), systemic inflammation [modified Glasgow prognostic score (mGPS)] and body composition [skeletal muscle index (SMI) and skeletal muscle density (SMD)] were examined in relation to clinical outcomes in patients undergoing surgery for colorectal cancer (CRC).
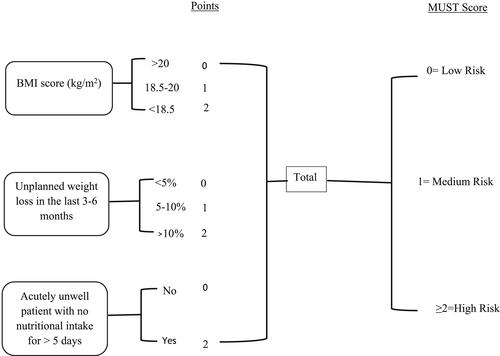
Data were collected for stages I–III CRC patients from prospectively maintained data base at the academic department of surgery, Glasgow Royal Infirmary. From the initial sample of 1046, pre-admission MUST score was available in 984 patients. The classification into low malnutrition risk (MUST = 0, n = 810) and moderate to high malnutrition risk (MUST 1 to ≥2, n = 174) groups and their relationship to systemic inflammatory response and body composition (SMI and SMD) with clinical outcomes were examined using univariate and multivariate analyses.
Compared with those patients at low nutrition risk (MUST = 0), patients at moderate to high malnutrition risk (MUST 1 to ≥2) had an elevated mGPS (P < 0.001), neutrophil lymphocyte ratio (NLR) (P < 0.001), low SMI (P ≤ 0.001) and low SMD (P = 0.015). MUST was an important prognostic factor for length of hospital stay (P < 0.001) and 3 years overall survival (P < 0.001).
In low malnutrition risk patients (MUST = 0), those who were systemically inflammed (mGPS 1/2, n = 187), had an elevated NLR (P < 0.001), low SMI (P < 0.001), low SMD (P < 0.01), increased post-operative complications (P < 0.05), longer hospital stay >7 days (P < 0.001), and poorer 3 years survival (P < 0.05) compared with those who were not systemically inflamed. On multivariate analysis, American Society of Anaesthesiologist (ASA) score (P < 0.05) and mGPS (P < 0.05) were independently associated with increased risk of clinical complications. ASA, mGPS, and NLR were independently associated with prolonged hospital stay (P < 0.05, P < 0.05, and P < 0.001, respectively). ASA, tumour, node, metastasis stage, and mGPS were independently associated with overall survival (P < 0.01, P < 0.001, and P < 0.05, respectively).
In medium-risk to high-risk patients (MUST = 1/2), those who were systemically inflamed (mGPS 1/2, n = 75) had higher ASA (P < 0.05), elevated NLR (P < 0.01), low SMI (P = 0.05) and low SMD (P < 0.05), increased length of hospital stay (P < 0.05), and poorer 3 years survival (P < 0.01), compared with those who were not systemically inflamed.
A small proportion of patients with primary operable CRC was at nutrition risk as defined by MUST alone in both low risk nutrition patients and medium/high risk nutrition patients. The systemic inflammatory response was associated with lower SMI, lower SMD, and poor clinical outcomes. The systemic inflammatory response is an important measure in the nutritional assessment of patients undergoing surgery for CRC.