The differential diagnosis of mucoepidermoid carcinoma (MEC) from neoplasm undergoing mucinous features brings more pitfalls to pathologists. Combining specific MAML2 gene rearrangement and histological characteristics may be the solution.
Twenty-five tumors with mucinous components were selected for differential diagnosis of MEC. All the cases were detected for MAML2 gene rearrangement. The cases diagnosed as MEC were classified into four variants: classic, oncocytic, Warthin-like, and nonclassified, and they were graded using the Brandwein system. The histological characteristics of non-MECs were summarized for differential diagnosis. Univariate survival analysis was performed on MECs.
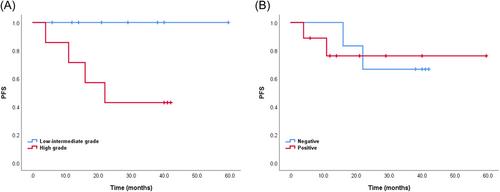
There were 16 MECs; 62.5% were MAML2 rearranged. For the low-, intermediate-, and high-grade MECs, the rate of rearrangement was 83.3%, 100%, and 28.6%, respectively. Both the oncocytic and Warthin-like MECs were MAML2 rearranged. For the classic and nonclassified MECs without MAML2 rearrangement, non-keratinized squamoid cells and distinctive mucinous cells were essential diagnostic criteria. On survival analysis, all the disease progression occurred in high-grade MECs (p = 0.038). Nine cases were diagnosed as non-MECs: pleomorphic adenoma with mucinous metaplasia showed no ex-capsular involvement; metaplastic Warthin tumor appeared with overt keratinization and residual oncocytic bilayered epithelium; mix squamous cell and glandular papilloma showed an endobronchial papillary growing pattern; adenosquamous carcinoma was accompanied by squamous carcinoma in situ of the overlying mucosa. All the non-MECs were negative for MAML2 rearrangement.
The application of combining MAML2 rearrangement and histological characteristics is helpful in the differential diagnosis between MEC and other tumors with mucinous components.