Preoperative autologous blood donation (PAD) is used for elective surgical procedures with a predictable blood loss. But a downward trend in PAD is due to the fact that patients with preoperative whole blood donation or two-unit red cell apheresis cannot avoid receiving allogenic blood during intensive surgery. To improve the clinical application of PAD, this study explores the feasibility of large-volume autologous red blood cells (RBCs) donation by a pilot trial in a small cohort of Chinese.
This was a single-center, prospective study and 16 male volunteers were enrolled from May to October in 2020. Each volunteer donated 627.25 ± 109.74 mL (mean ± SD) RBC with apheresis machine or manually, and received 800 mg of intravenous iron in four divided doses. Blood pressure, oxygen saturation (SpO2), respiratory rate and heart rate were monitored throughout the procedure. The RBC count, hemoglobin (Hb) concentration, hematocrit (Hct), reticulocyte count, erythropoietin (Epo), serum iron, total iron binding capacity (TIBC), transferrin saturation, transferrin, and ferritin were dynamically detected and analyzed before and 8 weeks after blood donation.
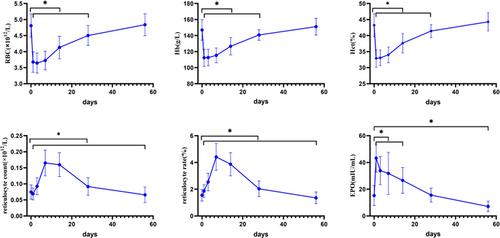
There was no differences in SpO2, systolic and diastolic blood pressure before and after blood collection (P ≥ .05). The heart rate and respiratory rate after donation were slightly lower than those before (P < .05). The level of RBC, Hb concentration and Hct fell to a nadir on Day 3 (pre-donation vs post-donation on Day 3: RBC 4.81 ± 0.36*1012 /L vs 3.65 ± 0.31, P < .05; Hb 148.59 ± 11.92 g/L vs 113.19 ± 10.43 g/L, P < .05; Hct 44.08 ± 3.06% vs 33.38 ± 2.57%, P < .05) and recovered to the pre-donation levels at the eighth week post donation (pre-donation vs post-donation at the eighth week: RBC 4.81 ± 0.36*1012 /L vs 4.84 ± 0.34*1012 /L, P ≥ .05; Hb 148.59 ± 11.92 g/L vs 150.91 ± 11.75 g/L, P ≥ .05; Hct 44.08% ± 3.06% vs 43.86 ± 3.06%, P ≥ .05). Epo and the reticulocyte count reached the peak values on Days 1 and 7, respectively (Epo: D0 15.30 ± 7.47 mlU/ML vs D1 43.26 ± 10.52 mlU/ML, P < .05; reticulocyte count: D0 0.07 ± 0.02*109/L vs D7 0.17 ± 0.04*109 /L, P < .05). The red cell net profits on Day 7, the second, fourth and eighth week postdonation were 160.39 ± 144.33 mL, 387.59 ± 128.74 mL, 530.95 ± 120.37 mL, and 614.18 ± 120.10 mL, and accounted for 27.47% ± 24.70%, 63.75% ± 24.91%, 86.20% ± 22.99%, and 99.20% ± 19.19% of RBC donation, respectively. The levels of serum iron, serum ferritin, and transferrin saturation increased during the first week because of the supplement of intravenous iron, and then gradually decreased and declined to the baseline at the end of the study period at the eighth week.
The large-volume autologous RBCs donation of 600 mL is proved safe in our study. Combination support of normal saline to maintain blood volume and intravenous iron supplementation may ensure the safety and effectiveness of large-volume RBC apheresis.