下载PDF
{"title":"间质性膀胱炎:弱子宫骶韧带不能支持内脏丛和膀胱拉伸受体的结果,因此可能治愈吗?","authors":"Peter Petros","doi":"10.5213/inj.2142366.183","DOIUrl":null,"url":null,"abstract":"Copyright © 2022 Korean Continence Society This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Corresponding author: Peter Petros https://orcid.org/0000-0002-9611-3258 University of Western Australia School of Mechanical and Mathematical Engineering, Perth, Australia Email: pp@kvinno.com *Current status: retired pelvic floor surgeon. Submitted: November 29, 2021 / Accepted after revision: June 9, 2022 To the editor, I read the state-of-the-art review of interstitial cystitis/bladder pain syndrome (IC/BPS) by Ueda et al. [1] with great interest. An erudite, scholarly paper, it states there is a crisis as regards IC—namely, there has been no progress for 25 years. The authors concluded [1], “Thus, there can be no bright future for IC/BPS without these 3 steps: (1) understanding the symptoms, (2) detecting abnormal findings in or outside the bladder, and (3) verifying that the abnormality is the cause of the symptoms” [1]. This commentary aims to address their statements, first by introducing an important discovery to International Neurourology Journal readers, Dr. Scheffler’s histologically validated cure of IC/BPS with Hunner ulcer (nonulcerating) [2], and then by discussing its implications relevant to those 3 statements [1]. Scheffler set out to manage a 73-year-old woman with classical posterior fornix syndrome (PFS) symptoms—predictably co-occurring chronic pelvic pain (CPP), urge, abnormal emptying/retention, nocturia, and frequency—caused by laxity of the uterosacral ligaments (USLs) and cured by repair thereof [3], not IC, by repair of cardinal ligaments and USLs, which is the standard cure for PFS [3]. To test whether any relationship exists between PFS and IC [2], we revisited previous data from 46 women with CPP and 171 bladder symptoms, treated for PFS with tissue fixation system (TFS) mini-sling surgery, who fit the International Continence Society (ICS) definition of IC [4]. Their workup [5], included the validated Integral Theory System Questionnaire, preoperative and postoperative urodynamics evaluations, and speculum testing (Fig. 1). The cure rates [5] were 76% for CPP, 74% for urge incontinence, 80% for abnormal emptying/retention, 75% for nocturia 75%, and 50% for frequency. Two women had glomerulations. None had Hunner ulcers. In another study by Wagenlehner et al. [6], among 1,420 women with prolapse and PFS symptoms treated by 2 different posterior sling operations, 599 had CPP, 1,179 had bladder symptoms, and 162 had fecal incontinence. A TFS study by Liedl et al. [7], found that 194 women had CPP, with 881 bladder symptoms that were variously cured. Other data showed small pain/urge symptom deterioration at 5 years [8]. The cure of CPP and bladder symptoms [6-8] was in accordance with the ICS definition of IC. All studies [6-8] fit the IC definition [4], but no Hunner ulcers were reported in any study. How is it that PFS studies [2,5-8] following the integral theory paradigm [9] have reported pain/urge cure by USL repair, while scholarly reviews have stated that the pathogenesis of IC is unknown and there is no cure [1]? The answer may be found in Thomas Kuhn’s famous book, The Structure of Scientific Revolutions [10]. Kuhn [10] states that solutions to chronic problems in science do not arrive gradually. Instead, they arrive in leaps. They are usually disruptive and only become “normal science” when there is a crisis. The leap in the science behind the IC cure, was the integral theory of female urinary incontinence, which was first published in 1990 [9]. It stated that stress urinary incontinence (SUI) and urge Letter to the Editor","PeriodicalId":14466,"journal":{"name":"International Neurourology Journal","volume":"26 4","pages":"349-351"},"PeriodicalIF":1.8000,"publicationDate":"2022-12-01","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://ftp.ncbi.nlm.nih.gov/pub/pmc/oa_pdf/98/e5/inj-2142366-183.PMC9816441.pdf","citationCount":"0","resultStr":"{\"title\":\"Interstitial Cystitis: A Consequence of Weakened Uterosacral Ligaments Failing to Support Visceral Plexuses and Bladder Stretch Receptors, and Therefore Potentially Curable?\",\"authors\":\"Peter Petros\",\"doi\":\"10.5213/inj.2142366.183\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"Copyright © 2022 Korean Continence Society This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Corresponding author: Peter Petros https://orcid.org/0000-0002-9611-3258 University of Western Australia School of Mechanical and Mathematical Engineering, Perth, Australia Email: pp@kvinno.com *Current status: retired pelvic floor surgeon. Submitted: November 29, 2021 / Accepted after revision: June 9, 2022 To the editor, I read the state-of-the-art review of interstitial cystitis/bladder pain syndrome (IC/BPS) by Ueda et al. [1] with great interest. An erudite, scholarly paper, it states there is a crisis as regards IC—namely, there has been no progress for 25 years. The authors concluded [1], “Thus, there can be no bright future for IC/BPS without these 3 steps: (1) understanding the symptoms, (2) detecting abnormal findings in or outside the bladder, and (3) verifying that the abnormality is the cause of the symptoms” [1]. This commentary aims to address their statements, first by introducing an important discovery to International Neurourology Journal readers, Dr. Scheffler’s histologically validated cure of IC/BPS with Hunner ulcer (nonulcerating) [2], and then by discussing its implications relevant to those 3 statements [1]. Scheffler set out to manage a 73-year-old woman with classical posterior fornix syndrome (PFS) symptoms—predictably co-occurring chronic pelvic pain (CPP), urge, abnormal emptying/retention, nocturia, and frequency—caused by laxity of the uterosacral ligaments (USLs) and cured by repair thereof [3], not IC, by repair of cardinal ligaments and USLs, which is the standard cure for PFS [3]. To test whether any relationship exists between PFS and IC [2], we revisited previous data from 46 women with CPP and 171 bladder symptoms, treated for PFS with tissue fixation system (TFS) mini-sling surgery, who fit the International Continence Society (ICS) definition of IC [4]. Their workup [5], included the validated Integral Theory System Questionnaire, preoperative and postoperative urodynamics evaluations, and speculum testing (Fig. 1). The cure rates [5] were 76% for CPP, 74% for urge incontinence, 80% for abnormal emptying/retention, 75% for nocturia 75%, and 50% for frequency. Two women had glomerulations. None had Hunner ulcers. In another study by Wagenlehner et al. [6], among 1,420 women with prolapse and PFS symptoms treated by 2 different posterior sling operations, 599 had CPP, 1,179 had bladder symptoms, and 162 had fecal incontinence. A TFS study by Liedl et al. [7], found that 194 women had CPP, with 881 bladder symptoms that were variously cured. Other data showed small pain/urge symptom deterioration at 5 years [8]. The cure of CPP and bladder symptoms [6-8] was in accordance with the ICS definition of IC. All studies [6-8] fit the IC definition [4], but no Hunner ulcers were reported in any study. How is it that PFS studies [2,5-8] following the integral theory paradigm [9] have reported pain/urge cure by USL repair, while scholarly reviews have stated that the pathogenesis of IC is unknown and there is no cure [1]? The answer may be found in Thomas Kuhn’s famous book, The Structure of Scientific Revolutions [10]. Kuhn [10] states that solutions to chronic problems in science do not arrive gradually. Instead, they arrive in leaps. They are usually disruptive and only become “normal science” when there is a crisis. The leap in the science behind the IC cure, was the integral theory of female urinary incontinence, which was first published in 1990 [9]. It stated that stress urinary incontinence (SUI) and urge Letter to the Editor\",\"PeriodicalId\":14466,\"journal\":{\"name\":\"International Neurourology Journal\",\"volume\":\"26 4\",\"pages\":\"349-351\"},\"PeriodicalIF\":1.8000,\"publicationDate\":\"2022-12-01\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://ftp.ncbi.nlm.nih.gov/pub/pmc/oa_pdf/98/e5/inj-2142366-183.PMC9816441.pdf\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"International Neurourology Journal\",\"FirstCategoryId\":\"3\",\"ListUrlMain\":\"https://doi.org/10.5213/inj.2142366.183\",\"RegionNum\":3,\"RegionCategory\":\"医学\",\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q3\",\"JCRName\":\"UROLOGY & NEPHROLOGY\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"International Neurourology Journal","FirstCategoryId":"3","ListUrlMain":"https://doi.org/10.5213/inj.2142366.183","RegionNum":3,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q3","JCRName":"UROLOGY & NEPHROLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Interstitial Cystitis: A Consequence of Weakened Uterosacral Ligaments Failing to Support Visceral Plexuses and Bladder Stretch Receptors, and Therefore Potentially Curable?
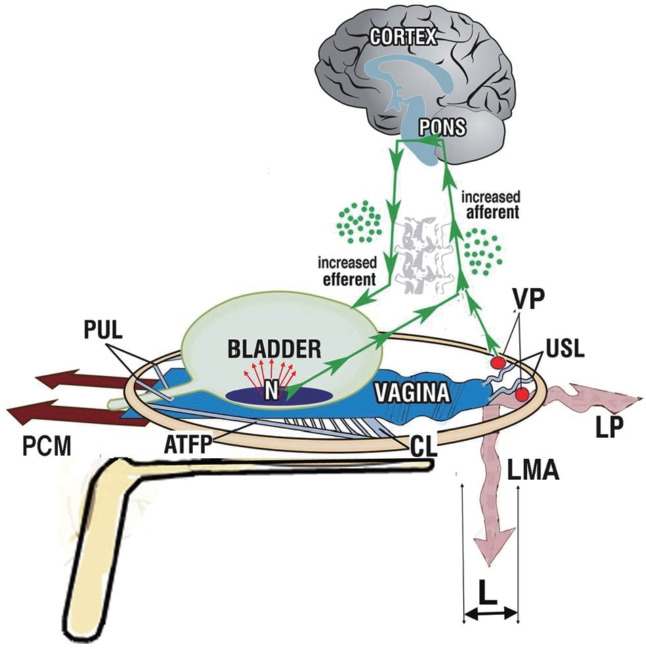
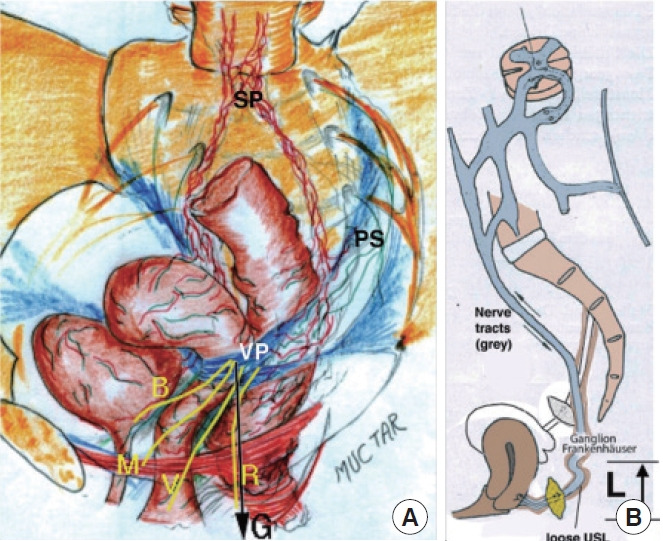
Copyright © 2022 Korean Continence Society This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Corresponding author: Peter Petros https://orcid.org/0000-0002-9611-3258 University of Western Australia School of Mechanical and Mathematical Engineering, Perth, Australia Email: pp@kvinno.com *Current status: retired pelvic floor surgeon. Submitted: November 29, 2021 / Accepted after revision: June 9, 2022 To the editor, I read the state-of-the-art review of interstitial cystitis/bladder pain syndrome (IC/BPS) by Ueda et al. [1] with great interest. An erudite, scholarly paper, it states there is a crisis as regards IC—namely, there has been no progress for 25 years. The authors concluded [1], “Thus, there can be no bright future for IC/BPS without these 3 steps: (1) understanding the symptoms, (2) detecting abnormal findings in or outside the bladder, and (3) verifying that the abnormality is the cause of the symptoms” [1]. This commentary aims to address their statements, first by introducing an important discovery to International Neurourology Journal readers, Dr. Scheffler’s histologically validated cure of IC/BPS with Hunner ulcer (nonulcerating) [2], and then by discussing its implications relevant to those 3 statements [1]. Scheffler set out to manage a 73-year-old woman with classical posterior fornix syndrome (PFS) symptoms—predictably co-occurring chronic pelvic pain (CPP), urge, abnormal emptying/retention, nocturia, and frequency—caused by laxity of the uterosacral ligaments (USLs) and cured by repair thereof [3], not IC, by repair of cardinal ligaments and USLs, which is the standard cure for PFS [3]. To test whether any relationship exists between PFS and IC [2], we revisited previous data from 46 women with CPP and 171 bladder symptoms, treated for PFS with tissue fixation system (TFS) mini-sling surgery, who fit the International Continence Society (ICS) definition of IC [4]. Their workup [5], included the validated Integral Theory System Questionnaire, preoperative and postoperative urodynamics evaluations, and speculum testing (Fig. 1). The cure rates [5] were 76% for CPP, 74% for urge incontinence, 80% for abnormal emptying/retention, 75% for nocturia 75%, and 50% for frequency. Two women had glomerulations. None had Hunner ulcers. In another study by Wagenlehner et al. [6], among 1,420 women with prolapse and PFS symptoms treated by 2 different posterior sling operations, 599 had CPP, 1,179 had bladder symptoms, and 162 had fecal incontinence. A TFS study by Liedl et al. [7], found that 194 women had CPP, with 881 bladder symptoms that were variously cured. Other data showed small pain/urge symptom deterioration at 5 years [8]. The cure of CPP and bladder symptoms [6-8] was in accordance with the ICS definition of IC. All studies [6-8] fit the IC definition [4], but no Hunner ulcers were reported in any study. How is it that PFS studies [2,5-8] following the integral theory paradigm [9] have reported pain/urge cure by USL repair, while scholarly reviews have stated that the pathogenesis of IC is unknown and there is no cure [1]? The answer may be found in Thomas Kuhn’s famous book, The Structure of Scientific Revolutions [10]. Kuhn [10] states that solutions to chronic problems in science do not arrive gradually. Instead, they arrive in leaps. They are usually disruptive and only become “normal science” when there is a crisis. The leap in the science behind the IC cure, was the integral theory of female urinary incontinence, which was first published in 1990 [9]. It stated that stress urinary incontinence (SUI) and urge Letter to the Editor