下载PDF
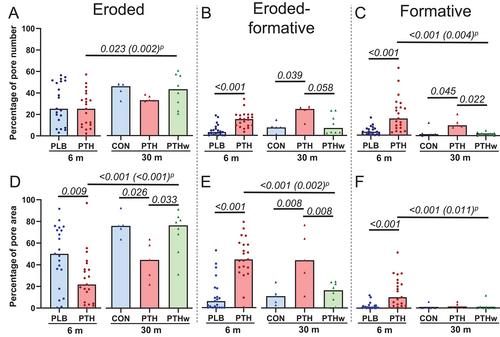
{"title":"接受 rhPTH(1-84) 治疗的甲状旁腺功能减退症患者骨皮质内骨重塑过程中的短暂活化和从侵蚀到形成的过渡得到改善","authors":"Pernille van Dijk Christiansen, Tanja Sikjær, Christina Møller Andreasen, Jesper Skovhus Thomsen, Annemarie Brüel, Ellen Margrethe Hauge, Jean-Marie Delaisse, Lars Rejnmark, Thomas Levin Andersen","doi":"10.1002/jbm4.10829","DOIUrl":null,"url":null,"abstract":"<p>In hypoparathyroidism, lack of parathyroid hormone (PTH) leads to low calcium levels and decreased bone remodeling. Treatment with recombinant human PTH (rhPTH) may normalize bone turnover. This study aimed to investigate whether rhPTH(1–84) continued to activate intracortical bone remodeling after 30 months and promoted the transition from erosion to formation and whether this effect was transitory when rhPTH(1–84) was discontinued. Cortical histomorphometry was performed on 60 bone biopsies from patients (aged 31 to 78 years) with chronic hypoparathyroidism randomized to either 100 μg rhPTH(1–84) a day (<i>n</i> = 21) (PTH) or similar placebo (<i>n</i> = 21) (PLB) for 6 months as add-on to conventional therapy. This was followed by an open-label extension, where patients extended their rhPTH(1–84) (PTH) (<i>n</i> = 5), continued conventional treatment (CON) (<i>n</i> = 5), or withdrew from rhPTH(1–84) and resumed conventional therapy (PTHw) for an additional 24 months (<i>n</i> = 8). Bone biopsies were collected at months 6 (<i>n</i> = 42) and 30 (<i>n</i> = 18). After 6 and 30 months, the overall cortical microarchitecture (cortical porosity, thickness, pore density, and mean pore diameter) in the PTH group did not differ from that of the PLB/CON and PTHw groups. Still, the PTH group had a significantly and persistently higher percentage of pores undergoing remodeling than the PLB/CON groups. A significantly higher percentage of these pores was undergoing bone formation in the PTH compared with the PLB/CON groups, whereas the percentage of pores with erosion only was not different. This resulted in a shift in the ratio between formative and eroded pores, reflecting a faster transition from erosion to formation in the PTH-treated patients. In the rhPTH(1–84) withdrawal group PTHw, the latter effects of PTH were completely reversed in comparison to those of the PLB/CON groups. In conclusion, rhPTH(1–84) replacement therapy in hypoparathyroidism patients promotes intracortical remodeling and its transition from erosion to formation without affecting the overall cortical microstructure. The effect persists for at least 30 months and is reversible when treatment is withdrawn. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 12","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-11-17","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10829","citationCount":"0","resultStr":"{\"title\":\"Transitory Activation and Improved Transition from Erosion to Formation within Intracortical Bone Remodeling in Hypoparathyroid Patients Treated with rhPTH(1–84)\",\"authors\":\"Pernille van Dijk Christiansen, Tanja Sikjær, Christina Møller Andreasen, Jesper Skovhus Thomsen, Annemarie Brüel, Ellen Margrethe Hauge, Jean-Marie Delaisse, Lars Rejnmark, Thomas Levin Andersen\",\"doi\":\"10.1002/jbm4.10829\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>In hypoparathyroidism, lack of parathyroid hormone (PTH) leads to low calcium levels and decreased bone remodeling. Treatment with recombinant human PTH (rhPTH) may normalize bone turnover. This study aimed to investigate whether rhPTH(1–84) continued to activate intracortical bone remodeling after 30 months and promoted the transition from erosion to formation and whether this effect was transitory when rhPTH(1–84) was discontinued. Cortical histomorphometry was performed on 60 bone biopsies from patients (aged 31 to 78 years) with chronic hypoparathyroidism randomized to either 100 μg rhPTH(1–84) a day (<i>n</i> = 21) (PTH) or similar placebo (<i>n</i> = 21) (PLB) for 6 months as add-on to conventional therapy. This was followed by an open-label extension, where patients extended their rhPTH(1–84) (PTH) (<i>n</i> = 5), continued conventional treatment (CON) (<i>n</i> = 5), or withdrew from rhPTH(1–84) and resumed conventional therapy (PTHw) for an additional 24 months (<i>n</i> = 8). Bone biopsies were collected at months 6 (<i>n</i> = 42) and 30 (<i>n</i> = 18). After 6 and 30 months, the overall cortical microarchitecture (cortical porosity, thickness, pore density, and mean pore diameter) in the PTH group did not differ from that of the PLB/CON and PTHw groups. Still, the PTH group had a significantly and persistently higher percentage of pores undergoing remodeling than the PLB/CON groups. A significantly higher percentage of these pores was undergoing bone formation in the PTH compared with the PLB/CON groups, whereas the percentage of pores with erosion only was not different. This resulted in a shift in the ratio between formative and eroded pores, reflecting a faster transition from erosion to formation in the PTH-treated patients. In the rhPTH(1–84) withdrawal group PTHw, the latter effects of PTH were completely reversed in comparison to those of the PLB/CON groups. In conclusion, rhPTH(1–84) replacement therapy in hypoparathyroidism patients promotes intracortical remodeling and its transition from erosion to formation without affecting the overall cortical microstructure. The effect persists for at least 30 months and is reversible when treatment is withdrawn. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>\",\"PeriodicalId\":14611,\"journal\":{\"name\":\"JBMR Plus\",\"volume\":\"7 12\",\"pages\":\"\"},\"PeriodicalIF\":3.4000,\"publicationDate\":\"2023-11-17\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10829\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"JBMR Plus\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10829\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q2\",\"JCRName\":\"ENDOCRINOLOGY & METABOLISM\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10829","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
引用
批量引用