下载PDF
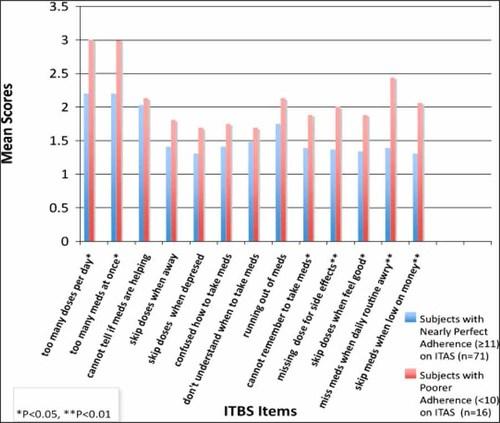
{"title":"高危成人肾移植受者免疫抑制药物依从性的障碍","authors":"Melissa Constantiner BA, Daniel Cukor PhD","doi":"10.1002/dat.20536","DOIUrl":null,"url":null,"abstract":"<div>\n \n \n <section>\n \n <h3> BACKGROUND</h3>\n \n <p>Non-adherence to immunosuppressive medication in renal transplant recipients is a primary cause of kidney rejection. However, little is known about the reasons transplant patients are non-adherent. We report on the specific barriers to medication adherence in 94 kidney transplant recipients from a medical center in Brooklyn, New York.</p>\n </section>\n \n <section>\n \n <h3> METHODS</h3>\n \n <p>Transplant patients waiting for their monthly medical appointment completed questionnaires relating to their adherence, level of depression, barriers to medication taking, and beliefs in their abilities to take their medication as prescribed.</p>\n </section>\n \n <section>\n \n <h3> RESULTS</h3>\n \n <p>The particular barriers that were most associated with lower levels of adherence were too many doses per day, too many pills per dose, having to remember to take medication, perceived side effects of medication, skipping a dose to feel good, falling out of a daily routine, and being short of money. The overall level of barriers that the sample endorsed was associated with increased depression (r = 0.209, <i>p</i> = 0.049) and decreased medi-cation self-efficacy (r = −0.300, <i>p</i> = 0.004). An elevation in the “unintentional” factor of the barriers scale was significantly associated with depression (r = 0.211, <i>p</i> = 0.046), but not directly with adherence. The “deliberate” factor was associated with non-adherence (r = −0.21, <i>p</i> < 0.05) but not depression (r = 0.173, <i>p</i> > 0.05)</p>\n </section>\n \n <section>\n \n <h3> CONCLUSIONS</h3>\n \n <p>There may be two reasons transplant recipients are non-adherent to prescribed medications. One set of barriers is related to deliberately choosing to skip doses, and the other set is related to inadvertent or uncontrollable situations. Interventions designed to promote adherence in this population should address both pathways. Dial. Transplant. © 2011 Wiley Periodicals, Inc.</p>\n </section>\n </div>","PeriodicalId":51012,"journal":{"name":"Dialysis & Transplantation","volume":"40 2","pages":"60-66"},"PeriodicalIF":0.0000,"publicationDate":"2011-02-15","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://sci-hub-pdf.com/10.1002/dat.20536","citationCount":"25","resultStr":"{\"title\":\"Barriers to immunosuppressive medication adherence in high-risk adult renal transplant recipients\",\"authors\":\"Melissa Constantiner BA, Daniel Cukor PhD\",\"doi\":\"10.1002/dat.20536\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<div>\\n \\n \\n <section>\\n \\n <h3> BACKGROUND</h3>\\n \\n <p>Non-adherence to immunosuppressive medication in renal transplant recipients is a primary cause of kidney rejection. However, little is known about the reasons transplant patients are non-adherent. We report on the specific barriers to medication adherence in 94 kidney transplant recipients from a medical center in Brooklyn, New York.</p>\\n </section>\\n \\n <section>\\n \\n <h3> METHODS</h3>\\n \\n <p>Transplant patients waiting for their monthly medical appointment completed questionnaires relating to their adherence, level of depression, barriers to medication taking, and beliefs in their abilities to take their medication as prescribed.</p>\\n </section>\\n \\n <section>\\n \\n <h3> RESULTS</h3>\\n \\n <p>The particular barriers that were most associated with lower levels of adherence were too many doses per day, too many pills per dose, having to remember to take medication, perceived side effects of medication, skipping a dose to feel good, falling out of a daily routine, and being short of money. The overall level of barriers that the sample endorsed was associated with increased depression (r = 0.209, <i>p</i> = 0.049) and decreased medi-cation self-efficacy (r = −0.300, <i>p</i> = 0.004). An elevation in the “unintentional” factor of the barriers scale was significantly associated with depression (r = 0.211, <i>p</i> = 0.046), but not directly with adherence. The “deliberate” factor was associated with non-adherence (r = −0.21, <i>p</i> < 0.05) but not depression (r = 0.173, <i>p</i> > 0.05)</p>\\n </section>\\n \\n <section>\\n \\n <h3> CONCLUSIONS</h3>\\n \\n <p>There may be two reasons transplant recipients are non-adherent to prescribed medications. One set of barriers is related to deliberately choosing to skip doses, and the other set is related to inadvertent or uncontrollable situations. Interventions designed to promote adherence in this population should address both pathways. Dial. Transplant. © 2011 Wiley Periodicals, Inc.</p>\\n </section>\\n </div>\",\"PeriodicalId\":51012,\"journal\":{\"name\":\"Dialysis & Transplantation\",\"volume\":\"40 2\",\"pages\":\"60-66\"},\"PeriodicalIF\":0.0000,\"publicationDate\":\"2011-02-15\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://sci-hub-pdf.com/10.1002/dat.20536\",\"citationCount\":\"25\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"Dialysis & Transplantation\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/dat.20536\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"\",\"JCRName\":\"\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"Dialysis & Transplantation","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/dat.20536","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"","JCRName":"","Score":null,"Total":0}
引用次数: 25
引用
批量引用