下载PDF
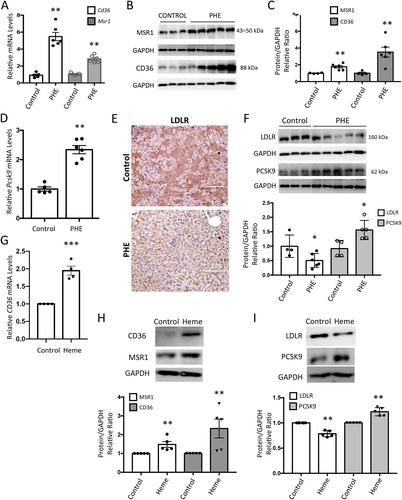
{"title":"血管内溶血触发NAFLD的特点是脂质代谢的解除和脂质吞噬阻断","authors":"Sandra Rayego-Mateos, José Luis Morgado-Pascual, Cristina García-Caballero, Iolanda Lazaro, Aleix Sala-Vila, Lucas Opazo-Rios, Sebastian Mas-Fontao, Jesús Egido, Marta Ruiz-Ortega, Juan Antonio Moreno","doi":"10.1002/path.6161","DOIUrl":null,"url":null,"abstract":"<p>Intravascular hemolysis is a common feature of different clinical entities, including sickle cell disease and malaria. Chronic hemolytic disorders are associated with hepatic damage; however, it is unknown whether heme disturbs lipid metabolism and promotes liver steatosis, thereby favoring the progression to nonalcoholic fatty liver disease (NAFLD). Using an experimental model of acute intravascular hemolysis, we report here the presence of liver injury in association with microvesicular lipid droplet deposition. Hemolysis promoted serum hyperlipidemia and altered intrahepatic triglyceride fatty acid composition, with increments in oleic, palmitoleic, and palmitic acids. These findings were related to augmented expression of transporters involved in fatty acid uptake (CD36 and MSR1) and deregulation of LDL transport, as demonstrated by decreased levels of LDL receptor and increased PCSK9 expression. Hemolysis also upregulated hepatic enzymes associated with cholesterol biosynthesis (SREBP2, HMGC1, LCAT, SOAT1) and transcription factors regulating lipid metabolism (SREBP1). Increased LC3II/LC3I ratio and p62/SQSTM1 protein levels were reported in mice with intravascular hemolysis and hepatocytes stimulated with heme, indicating a blockade of lipophagy. In cultured hepatocytes, cell pretreatment with the autophagy inductor rapamycin diminished heme-mediated toxicity and accumulation of lipid droplets. In conclusion, intravascular hemolysis enhances liver damage by exacerbating lipid accumulation and blocking the lipophagy pathway, thereby promoting NAFLD. These new findings have a high translational potential as a novel NAFLD-promoting mechanism in individuals suffering from severe hemolysis episodes. © 2023 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"261 2","pages":"169-183"},"PeriodicalIF":5.6000,"publicationDate":"2023-08-09","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6161","citationCount":"0","resultStr":"{\"title\":\"Intravascular hemolysis triggers NAFLD characterized by a deregulation of lipid metabolism and lipophagy blockade\",\"authors\":\"Sandra Rayego-Mateos, José Luis Morgado-Pascual, Cristina García-Caballero, Iolanda Lazaro, Aleix Sala-Vila, Lucas Opazo-Rios, Sebastian Mas-Fontao, Jesús Egido, Marta Ruiz-Ortega, Juan Antonio Moreno\",\"doi\":\"10.1002/path.6161\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>Intravascular hemolysis is a common feature of different clinical entities, including sickle cell disease and malaria. Chronic hemolytic disorders are associated with hepatic damage; however, it is unknown whether heme disturbs lipid metabolism and promotes liver steatosis, thereby favoring the progression to nonalcoholic fatty liver disease (NAFLD). Using an experimental model of acute intravascular hemolysis, we report here the presence of liver injury in association with microvesicular lipid droplet deposition. Hemolysis promoted serum hyperlipidemia and altered intrahepatic triglyceride fatty acid composition, with increments in oleic, palmitoleic, and palmitic acids. These findings were related to augmented expression of transporters involved in fatty acid uptake (CD36 and MSR1) and deregulation of LDL transport, as demonstrated by decreased levels of LDL receptor and increased PCSK9 expression. Hemolysis also upregulated hepatic enzymes associated with cholesterol biosynthesis (SREBP2, HMGC1, LCAT, SOAT1) and transcription factors regulating lipid metabolism (SREBP1). Increased LC3II/LC3I ratio and p62/SQSTM1 protein levels were reported in mice with intravascular hemolysis and hepatocytes stimulated with heme, indicating a blockade of lipophagy. In cultured hepatocytes, cell pretreatment with the autophagy inductor rapamycin diminished heme-mediated toxicity and accumulation of lipid droplets. In conclusion, intravascular hemolysis enhances liver damage by exacerbating lipid accumulation and blocking the lipophagy pathway, thereby promoting NAFLD. These new findings have a high translational potential as a novel NAFLD-promoting mechanism in individuals suffering from severe hemolysis episodes. © 2023 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>\",\"PeriodicalId\":232,\"journal\":{\"name\":\"The Journal of Pathology\",\"volume\":\"261 2\",\"pages\":\"169-183\"},\"PeriodicalIF\":5.6000,\"publicationDate\":\"2023-08-09\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6161\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"The Journal of Pathology\",\"FirstCategoryId\":\"3\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/path.6161\",\"RegionNum\":2,\"RegionCategory\":\"医学\",\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q1\",\"JCRName\":\"ONCOLOGY\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6161","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用