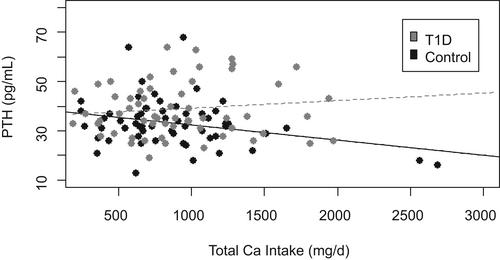
{"title":"Total Calcium Intake Is Associated With Trabecular Bone Density in Adolescent Girls With Type 1 Diabetes","authors":"Rylee K Saunders, Kathleen M Kilroe, Taïsha V. Joseph, Signe Caksa, Mary L Bouxsein, Madhusmita Misra, Deborah M Mitchell","doi":"10.1002/jbm4.10813","DOIUrl":null,"url":null,"abstract":"<p>Type 1 diabetes (T1D) confers an increased risk of fracture and is associated with lower bone mineral density (BMD) and altered microarchitecture compared with controls. Adequate calcium (Ca) intake promotes bone mineralization, thereby increasing BMD. The objective of this analysis was to evaluate the associations of total daily Ca intake with bone outcomes among youth with T1D. This was a cross-sectional analysis of girls ages 10–16 years with (<i>n</i> = 62) and without (<i>n</i> = 60) T1D. We measured Ca intake with a validated food-frequency questionnaire and BMD, microarchitecture, and strength estimates with dual-energy X-ray absorptiometry and high-resolution peripheral quantitative computed tomography. Total daily Ca intake did not differ between groups (950 ± 488 in T1D versus 862 ± 461 mg/d in controls, <i>p</i> = 0.306). Serum 25OHD was lower in T1D (26.3 ± 7.6 versus 32.6 ± 9.0 ng/mL, <i>p</i> = <0.001), and parathyroid hormone (PTH) was higher in T1D (38.9 ± 11 versus 33.4 ± 9.7 pg/mL, <i>p</i> = 0.004). Trabecular volumetric BMD and thickness at the tibia were lower in T1D (<i>p</i> = 0.013, <i>p</i> = 0.030). Ca intake correlated with trabecular BMD at the radius and tibia among T1D participants (β = 0.27, <i>p</i> = 0.047, and β = 0.28, <i>p</i> = 0.027, β = 0.28, respectively) but not among controls (p<sub>interaction</sub> = 0.009 at the radius, p<sub>interaction</sub> = 0.010 at the tibia). Similarly, Ca intake was associated with estimated failure load at the tibia in T1D but not control participants (<i>p</i> = 0.038, β = 0.18; p<sub>interaction</sub> = 0.051). We observed the expected negative association of Ca intake with parathyroid hormone in controls (<i>p</i> = 0.022, β = −0.29) but not in T1D participants (p<sub>interaction</sub> = 0.022). Average glycemia as measured by hemoglobin A1c did not influence the relationship of Ca and PTH among participants with T1D (p<sub>interaction</sub> = 0.138). These data suggest that youth with T1D may be particularly vulnerable to dietary Ca insufficiency. Increasing Ca intake may be an effective strategy to optimize bone health in this population. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC. on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":2.4000,"publicationDate":"2023-09-19","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10813","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10813","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
Abstract
Type 1 diabetes (T1D) confers an increased risk of fracture and is associated with lower bone mineral density (BMD) and altered microarchitecture compared with controls. Adequate calcium (Ca) intake promotes bone mineralization, thereby increasing BMD. The objective of this analysis was to evaluate the associations of total daily Ca intake with bone outcomes among youth with T1D. This was a cross-sectional analysis of girls ages 10–16 years with (n = 62) and without (n = 60) T1D. We measured Ca intake with a validated food-frequency questionnaire and BMD, microarchitecture, and strength estimates with dual-energy X-ray absorptiometry and high-resolution peripheral quantitative computed tomography. Total daily Ca intake did not differ between groups (950 ± 488 in T1D versus 862 ± 461 mg/d in controls, p = 0.306). Serum 25OHD was lower in T1D (26.3 ± 7.6 versus 32.6 ± 9.0 ng/mL, p = <0.001), and parathyroid hormone (PTH) was higher in T1D (38.9 ± 11 versus 33.4 ± 9.7 pg/mL, p = 0.004). Trabecular volumetric BMD and thickness at the tibia were lower in T1D (p = 0.013, p = 0.030). Ca intake correlated with trabecular BMD at the radius and tibia among T1D participants (β = 0.27, p = 0.047, and β = 0.28, p = 0.027, β = 0.28, respectively) but not among controls (pinteraction = 0.009 at the radius, pinteraction = 0.010 at the tibia). Similarly, Ca intake was associated with estimated failure load at the tibia in T1D but not control participants (p = 0.038, β = 0.18; pinteraction = 0.051). We observed the expected negative association of Ca intake with parathyroid hormone in controls (p = 0.022, β = −0.29) but not in T1D participants (pinteraction = 0.022). Average glycemia as measured by hemoglobin A1c did not influence the relationship of Ca and PTH among participants with T1D (pinteraction = 0.138). These data suggest that youth with T1D may be particularly vulnerable to dietary Ca insufficiency. Increasing Ca intake may be an effective strategy to optimize bone health in this population. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC. on behalf of American Society for Bone and Mineral Research.
1型糖尿病少女总钙摄入量与骨小梁密度相关
与对照组相比,1型糖尿病(T1D)会增加骨折的风险,并与较低的骨密度(BMD)和改变的微结构相关。充足的钙(Ca)摄入促进骨矿化,从而增加骨密度。本分析的目的是评估青少年T1D患者每日总钙摄入量与骨骼预后的关系。这是一项10-16岁女孩(n = 62)和不(n = 60) T1D的横断面分析。我们通过有效的食物频率问卷测量钙摄入量,并通过双能x射线吸收仪和高分辨率外围定量计算机断层扫描测量骨密度、微结构和强度。各组之间每日总钙摄入量没有差异(T1D组为950±488 mg/d,对照组为862±461 mg/d, p = 0.306)。T1D患者血清25OHD较低(26.3±7.6比32.6±9.0 ng/mL, p = <0.001), T1D患者甲状旁腺激素(PTH)较高(38.9±11比33.4±9.7 pg/mL, p = 0.004)。T1D患者骨小梁体积骨密度和胫骨厚度较低(p = 0.013, p = 0.030)。在T1D参与者中,钙摄入量与桡骨和胫骨骨小梁骨密度相关(β = 0.27, p = 0.047, β = 0.28, p = 0.027, β = 0.28),但在对照组中没有相关性(桡骨处p = 0.009,胫骨处p = 0.010)。同样,钙摄入量与T1D患者胫骨的估计衰竭负荷相关,但与对照组无关(p = 0.038, β = 0.18;p交互作用= 0.051)。我们观察到,在对照组中,钙摄入量与甲状旁腺激素呈预期的负相关(p = 0.022, β = - 0.29),但在T1D参与者中没有(p - interaction = 0.022)。糖化血红蛋白测量的平均血糖不影响T1D患者Ca和PTH的关系(相互作用= 0.138)。这些数据表明,患有T1D的青少年可能特别容易受到膳食钙不足的影响。增加钙的摄入可能是优化这一人群骨骼健康的有效策略。©2023作者。JBMR Plus由Wiley期刊有限责任公司代表美国骨与矿物研究协会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。