{"title":"Effects of Incretin Therapy on Skeletal Health in Type 2 Diabetes—A Systematic Review","authors":"Rikke Viggers, Nicklas Højgaard-hessellund Rasmussen, Peter Vestergaard","doi":"10.1002/jbm4.10817","DOIUrl":null,"url":null,"abstract":"<p>Diabetes poses a significant risk to bone health, with Type 1 diabetes (T1D) having a more detrimental impact than Type 2 diabetes (T2D). The group of hormones known as incretins, which includes gastric inhibitory peptide (GIP) and glucagon-like peptide 1 (GLP-1), play a role in regulating bowel function and insulin secretion during feeding. GLP-1 receptor agonists (GLP-1 RAs) are emerging as the primary treatment choice in T2D, particularly when atherosclerotic cardiovascular disease is present. Dipeptidyl peptidase 4 inhibitors (DPP-4is), although less potent than GLP-1 RAs, can also be used. Additionally, GLP-1 RAs, either alone or in combination with GIP, may be employed to address overweight and obesity. Since feeding influences bone turnover, a relationship has been established between incretins and bone health. To explore this relationship, we conducted a systematic literature review following the PRISMA guidelines. While some studies on cells and animals have suggested positive effects of incretins on bone cells, turnover, and bone density, human studies have yielded either no or limited and conflicting results regarding their impact on bone mineral density (BMD) and fracture risk. The effect on fracture risk may vary depending on the choice of comparison drug and the duration of follow-up, which was often limited in several studies. Nevertheless, GLP-1 RAs may hold promise for people with T2D who have multiple fracture risk factors and poor metabolic control. Furthermore, a potential new area of interest is the use of GLP-1 RAs in fracture prevention among overweight and obese people. Based on this systematic review, existing evidence remains insufficient to support a positive or a superior effect on bone health to reduce fracture risk in people with T2D. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":2.4000,"publicationDate":"2023-09-25","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10817","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10817","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
Abstract
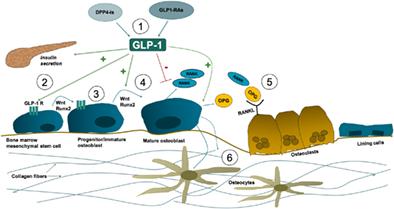
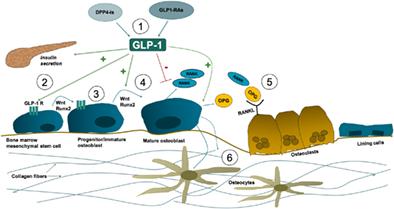
Diabetes poses a significant risk to bone health, with Type 1 diabetes (T1D) having a more detrimental impact than Type 2 diabetes (T2D). The group of hormones known as incretins, which includes gastric inhibitory peptide (GIP) and glucagon-like peptide 1 (GLP-1), play a role in regulating bowel function and insulin secretion during feeding. GLP-1 receptor agonists (GLP-1 RAs) are emerging as the primary treatment choice in T2D, particularly when atherosclerotic cardiovascular disease is present. Dipeptidyl peptidase 4 inhibitors (DPP-4is), although less potent than GLP-1 RAs, can also be used. Additionally, GLP-1 RAs, either alone or in combination with GIP, may be employed to address overweight and obesity. Since feeding influences bone turnover, a relationship has been established between incretins and bone health. To explore this relationship, we conducted a systematic literature review following the PRISMA guidelines. While some studies on cells and animals have suggested positive effects of incretins on bone cells, turnover, and bone density, human studies have yielded either no or limited and conflicting results regarding their impact on bone mineral density (BMD) and fracture risk. The effect on fracture risk may vary depending on the choice of comparison drug and the duration of follow-up, which was often limited in several studies. Nevertheless, GLP-1 RAs may hold promise for people with T2D who have multiple fracture risk factors and poor metabolic control. Furthermore, a potential new area of interest is the use of GLP-1 RAs in fracture prevention among overweight and obese people. Based on this systematic review, existing evidence remains insufficient to support a positive or a superior effect on bone health to reduce fracture risk in people with T2D. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.
肠促胰岛素治疗对2型糖尿病患者骨骼健康的影响——系统综述
糖尿病对骨骼健康构成重大风险,1型糖尿病(T1D)比2型糖尿病(T2D)具有更有害的影响。肠促胰岛素包括胃抑制肽(GIP)和胰高血糖素样肽1 (GLP-1),在喂养过程中调节肠道功能和胰岛素分泌。GLP-1受体激动剂(GLP-1 RAs)正在成为T2D的主要治疗选择,特别是当存在动脉粥样硬化性心血管疾病时。二肽基肽酶4抑制剂(DPP-4is)虽然不如GLP-1 RAs有效,但也可以使用。此外,GLP-1 RAs,单独或与GIP联合,可用于解决超重和肥胖。由于喂养影响骨转换,肠促胰岛素和骨骼健康之间的关系已经确立。为了探讨这种关系,我们按照PRISMA指南进行了系统的文献综述。虽然一些对细胞和动物的研究表明肠促胰岛素对骨细胞、周转率和骨密度有积极作用,但对人体的研究却没有发现肠促胰岛素对骨矿物质密度(BMD)和骨折风险的影响,或者结果有限,或者结果相互矛盾。对骨折风险的影响可能取决于比较药物的选择和随访时间,这在一些研究中往往是有限的。然而,GLP-1 RAs可能对有多种骨折危险因素和代谢控制不良的T2D患者有希望。此外,一个潜在的新领域是GLP-1 RAs在超重和肥胖人群中预防骨折的应用。基于这一系统综述,现有的证据仍然不足以支持对T2D患者的骨骼健康有积极或优越的影响,以降低骨折风险。©2023作者。JBMR Plus由Wiley期刊有限责任公司代表美国骨骼和矿物研究协会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。