Chronic kidney disease patients particularly with renal anaemia hyporesponsive to erythropoiesis-stimulating agents (ESAs) are at a greater risk of having skeletal muscle mass (SMM) loss. Hypoxia-inducible factor prolyl hydroxylase domain inhibitor (HIF-PHI), a novel therapeutic agent for renal anaemia, potentially promotes angiogenesis, muscle repair, and homeostasis. However, effects of HIF-PHIs on SMM remain unknown.
This retrospective observational cohort study enrolled 292 Japanese adults receiving maintenance haemodialysis at our dialysis centre. The dataset included 11 patients who received daprodustat for 6 months or longer during 1 December 2020 through 30 June 2022. From the previously published pooled cohort, we enrolled 281 participants from 1 August 2018 to 31 July 2019 prior to the approval of HIF-PHIs for renal anaemia. SMM was assessed using modified creatinine index (mg/kg/day) calculated by age, sex, serum creatinine, and single-pool Kt/V. Annual changes of SMM [ΔSMM (%)] were analysed with the least squares regression model and mixed-effects model during 6- to 12-month follow-up period.
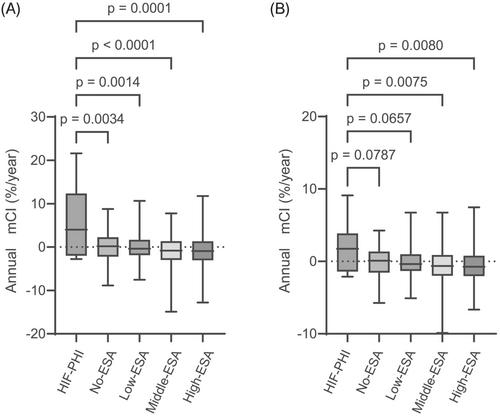
The median age of the participants was 63 years [interquartile range (IQR), 54–71 years], and 33% were female. The median ΔSMM levels (IQR) in the least squares regression model were 4.0% (−1.7% to 9.3%) in the HIF-PHI group, 0.20% (−2.1% to 2.1%) in the no ESA group, and −0.94% (−3.0% to 1.3%) in the high ESA group using darbepoetin equivalent to 20 μg or more per week. Those in the mixed-effects model were −1.7% (−1.2% to 3.8%), 0.09% (−1.4% to 1.3%), and −0.74% (−2.0% to 0.8%), respectively. The multivariable linear regression models revealed that HIF-PHI use was associated with greater ΔSMM compared with the high ESA group [coefficient, 3.737; 95% confidence interval (CI), 1.216–6.258 in the least squares regression model or coefficient, 1.635; 95% CI, 0.068–3.201 in the mixed-effects model, respectively].
HIF-PHI use led to greater ΔSMM in maintenance haemodialysis patients. HIF-PHIs may minimize loss of SMM in patients with end-stage kidney disease and renal anaemia.