Establishing interchangeable biomedical imaging-based measures to assess myosteatosis clinically may lead to the prevention of muscle wasting, yet neither a consensus measure nor a conversion between measures exists. Ultrasound echo intensity (EI) potentially assesses myosteatosis, but subcutaneous adipose tissue (SAT) thickness and user force application have been shown to influence EI. Although correction factors exist to adjust EI for SAT thickness, they are modelled against poor or no reference measures. Modelling EI corrections against a robust reference measure of myosteatosis, like magnetic resonance imaging (MRI)-based proton density fat fraction (PDFF), is necessary for EI's clinical application.
Healthy young adults, healthy older adults, and older adults undergoing treatment for lung cancer (n = 10 per group with 50% females) had PDFF and EI at 0, 5, 10, and 15 N measured on their right rectus femoris (RF). We compared EI, SAT thickness, and RF thickness between forces and groups and assessed the relationships between EI adjusted by four different correction factors and PDFF.
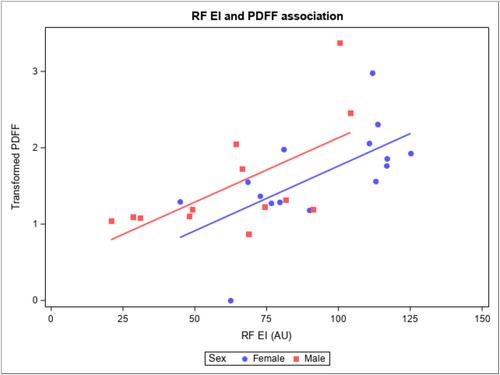
The mean age of our sample was 48.63 ± 19.68 years and had a body mass index of 25.21 ± 5.19 kg/m2. The correlation between PDFF and raw EI was r = 0.59 (P < 0.001) with negligible increases by previously published correction factors (Young: 0.62, P < 0.001; Neto Müller: 0.61, P < 0.001). EI, SAT thickness, and RF thickness did not significantly differ between forces (χ2 = 0.31, P = 0.957; χ2 = 2.39, P = 0.496; and χ2 = 7.75, P = 0.051, respectively). EI and PDFF were significantly lower among young healthy adults compared with older adult groups (χ2 = 12.88, P = 0.002, and χ2 = 9.13, P = 0.010, respectively).
EI is correlated with PDFF regardless of force with no improvement from previously published correction factors. Our results suggest that EI is clinically useful and influenced by fat content, yet correction factors must account for more than SAT thickness alone and require further investigation.