With increasing reports of accelerated and acute silicosis, PMF, and autoimmune disease among coal miners and silica-exposed countertop workers, we present previously incompletely-described pulmonary pathology of accelerated silicosis and correlations with mineralogy, radiography, and disease progression in 46 Texas oilfield pipe sandblasters who were biopsied between 1988 and 1995.
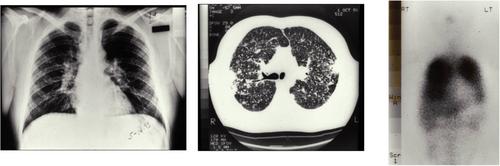
Worker examinations included pulmonary function tests, chest X-ray (CXR), high-resolution computed tomography (HRCT), and Gallium-67 scans. Quantitative mineralogic analysis of pulmonary parenchymal burden of silica, silicates, and metal particles used scanning electron microscopy with energy dispersive x-ray spectroscopy (SEM EDS).
Workers had clinical deterioration after <10 years exposure in dusty workplaces. Although initial CXR was normal in 54%, Gallium-67 scans were positive in 68% of those with normal CXR, indicating pulmonary inflammation. The histology of accelerated silicosis is diffuse interstitial infiltration of macrophages filled with weakly birefringent particles with or without silicotic nodules or alveolar proteinosis. Lung silica concentrations were among the highest in our database, showing a dose–response relationship with CXR, HRCT, and pathologic changes (macrophages, fibrosis, and silicotic nodules). Radiographic scores and diffusing capacity worsened during observation. Silica exposure was intensified, patients presented younger, with shorter exposure, more severe clinical abnormalities, higher lung particle burdens, and more rapid progression in a subset of patients exposed to recycled blasting sand.
Accelerated silicosis may present with a normal CXR despite significant histopathology. Multivariable analyses showed silica, and not other particles, is the driver of observed radiologic, physiologic, and histologic outcomes. Eliminating this preventable disease requires higher physician, public health, and societal awareness.