Breast cancer (BC), the most frequently diagnosed malignancy among women worldwide, presents a public health challenge and affects mortality rates. Breast-conserving therapy (BCT) is a common treatment, but the risk from residual disease necessitates radiotherapy. Digital mammography monitors treatment response by identifying post-operative and radiotherapy tissue alterations, but accurate assessment of mammographic density remains a challenge. This study used OpenBreast to measure percent density (PD), offering insights into changes in mammographic density before and after BCT with radiation therapy.
This retrospective analysis included 92 female patients with BC who underwent BCT, chemotherapy, and radiotherapy, excluding those who received hormonal therapy or bilateral BCT. Percent/percentage density measurements were extracted using OpenBreast, an automated software that applies computational techniques to density analyses. Data were analysed at baseline, 3 months, and 15 months post-treatment using standardised mean difference (SMD) with Cohen's d, chi-square, and paired sample t-tests. The predictive power of PD changes for BC was measured based on the receiver operating characteristic (ROC) curve analysis.
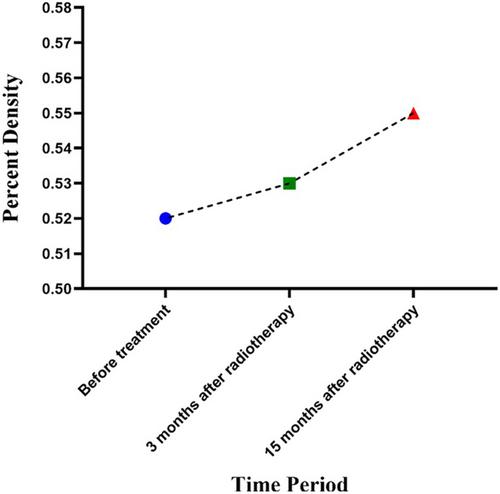
The mean age was 53.2 years. There were no significant differences in PD between the periods. Standardised mean difference analysis revealed no significant changes in the SMD for PD before treatment compared with 3- and 15-months post-treatment. Although PD increased numerically after radiotherapy, ROC analysis revealed optimal sensitivity at 15 months post-treatment for detecting changes in breast density.
This study utilised an automated breast density segmentation tool to assess the changes in mammographic density before and after BC treatment. No significant differences in the density were observed during the short-term follow-up period. However, the results suggest that quantitative density assessment could be valuable for long-term monitoring of treatment effects. The study underscores the necessity for larger and longitudinal studies to accurately measure and validate the effectiveness of quantitative methods in clinical BC management.