Polypharmacy is a primary risk factor for the prescription of potentially inappropriate medications (PIMs), drug–drug interactions (DDIs), and ultimately, adverse drug reactions (ADRs). Medication review and deprescribing represent effective strategies to simplify therapeutic regimens, minimize risks, and reduce PIM prescriptions. This systematic review and meta-analysis of experimental and observational studies aimed to evaluate the impact of different medication review and deprescribing interventions in hospitalized older patients.
Experimental and observational prospective cohort studies evaluating the clinical effects of medication review and deprescribing strategies in older hospitalized patients were searched in the bibliographic databases, PubMed, Embase, and Scopus, from inception until January 8, 2024. A narrative synthesis of the results was provided, along with a meta-analysis of dichotomous data (i.e., re-hospitalizations and mortality).
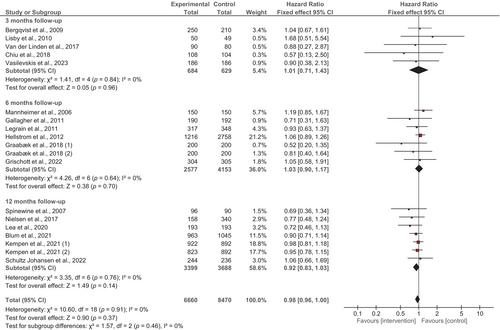
Overall, 21 randomized controlled trials, 7 non-randomized interventional studies, and 2 prospective cohort studies were included in the systematic review. Of these, 14 (46.7%) assessed medication appropriateness as the primary outcome, while the remaining evaluated clinical outcomes (e.g., length of hospital stay, hospital readmissions, emergency department visits, and incidence of ADRs) and/or quality of life. The meta-analysis revealed a slight but statistically significant 8% reduction in hospital readmissions (HR: 0.92; 95% CI: 0.85–0.99) following medication review and deprescribing, but no significant impact on mortality (HR: 0.98; 95% CI: 0.96–1.00). Of the 30 included studies, 21 were considered at high risk of bias, mostly due to potential deviations from intended interventions and randomization processes. The remaining nine studies had “some concerns” (eight studies) or were considered at “low” risk of bias (one study).
Medication review and deprescribing are associated with potential benefits in reducing hospital readmission rates among hospitalized older patients, particularly through the reduction of PIM prescriptions. The integration of thorough medication review and deprescribing protocols in hospital settings may improve post-discharge outcomes and reduce overall healthcare costs.