This work endeavored to examine the correlation between dietary choline intake and the odds of asthma, utilizing data from the National Health and Nutrition Examination Survey (NHANES).
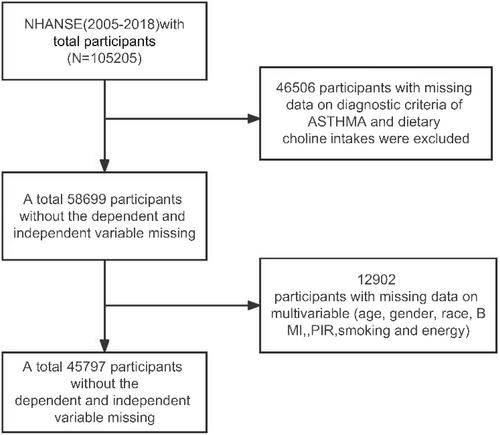
Aggregated data from seven cycles (2005–2018) in the NHANES database were utilized. The independent variable was dietary choline intake, and the dependent variable was asthma. The weighted logistic regression method was used to construct a model reflecting the relationship between these two factors. This work employed stratified analysis without adjusting for confounding factors and subgroup analysis with adjusted confounding factors to mine the association between dietary choline intake and asthma. Additionally, restricted cubic spline analysis examined nonlinear associations of the two in age subgroups.
Forty five thousand and seven hundreds ninety seven samples were included here. The model indicating the relationship between dietary choline intake and asthma was constructed (OR: 0.86, 95% CI: 0.79–0.93, p < 0.001). Stratified analysis indicated that the interaction terms of age (p < 0.001) and body mass index (BMI) (p = 0.002) with dietary choline intake significantly influenced the relationship model. In the adjusted models, accounting for demographic characteristics, poverty impact ratio, BMI, exposure to environmental tobacco smoke, and total energy intake, an increase in dietary choline intake significantly reduced the odds of asthma (OR: 0.79, 95% CI: 0.72–0.88, p < 0.001). Subgroup analyses based on age and BMI revealed a significant negative correlation between dietary choline intake and the odds of asthma in the adult population (OR: 0.76, 95% CI: 0.67–0.86, p < 0.001), as well as in individuals with a BMI between 25 and 30 kg/m2 (OR: 0.79, 95% CI: 0.63–0.99, p = 0.042), and those with a BMI >30 kg/m2 (OR: 0.73, 95% CI: 0.60–0.89, p = 0.002).
Dietary choline intake was significantly inversely correlated with asthma prevalence, especially in adults and overweight/obese individuals, suggesting that increasing choline intake may reduce asthma risk. Further research is needed to explore this relationship and provide tailored dietary recommendations for different age and BMI groups to enhance asthma prevention and management.