In Viet Nam, key populations (KPs) face barriers accessing HIV services. Virtual platforms can be leveraged to increase access for KPs, including for HIV self-testing (HIVST). This study compares reach and effectiveness of a web-based HIVST intervention from pilot to scale-up in Viet Nam.
A mixed-methods explanatory sequential design used cross-sectional and thematic analysis. The pilot launched in Can Tho in November 2020, followed by Hanoi and Nghe An in April 2021. Scale-up included Can Tho and Nghe An, with 21 novel provinces from April to December 2022.
After risk assessment, participants registered on the website, receiving HIVST (OraQuick®) by courier, peer educator or self-pick-up. Test result reporting and completing satisfaction surveys were encouraged.
Intervention reach was measured through numbers accessing the testing, disaggregated by demographics, and proportion of individuals reporting self-testing post-registration. Effectiveness was measured through numbers reporting self-test results, testing positive and linking to care, and testing negative and using HIVST to manage pre-exposure prophylaxis (PrEP) use. Thematic content analysis of free-text responses from the satisfaction survey synthesized quantitative outcomes.
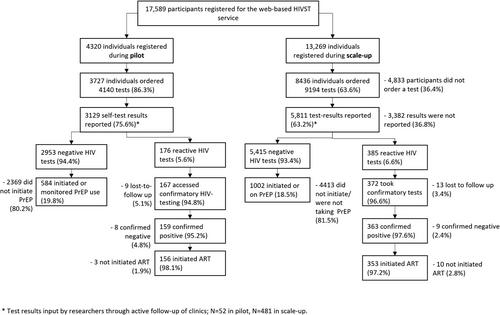
In total, 17,589 participants registered on the HIVST website; 11,332 individuals ordered 13,334 tests. Participants were generally young, aged <25 years (4309/11,332, 38.0%), male (9418/11,332, 83.1%) and men who have sex with men (6437/11,332, 56.8%). Nearly half were first-time testers (5069/11,332, 44.9%). Scale-up participants were two times more likely to be assigned female at birth (scale-up; 1595/8436, 18.9% compared to pilot; 392/3727, 10.5%, p < 0.001). Fewer test results were reported in scale-up compared with pilot (pilot: 3129/4140, 75.6%, scale-up: 5811/9194, 63.2%, p < 0.001).
6.3% of all tests were reactive (pilot: 176/3129, 5.6% reactive compared to scale-up: 385/5811, 6.6% reactive, p = 0.063); of which most linked to care (509/522, 97.5%). One-fifth of participants with a negative test initiated or continued PrEP (pilot; 19.8%, scale-up; 18.5%, p = 0.124). Thematic analysis suggested that community delivery models increased programmatic reach. Live chat may also be a suitable proxy for staff support to increase result reporting.
Web-based self-testing in Viet Nam reached people at elevated risk of HIV, facilitating uptake of anti-retroviral treatment and direct linkage to PrEP initiations. Further innovations such as the use of social-network testing services and incorporating features powered by artificial intelligence could increase the effectiveness and efficiency of the approach.