There is limited knowledge on the fabrication trueness and fit of additively or subtractively manufactured complete-arch implant-supported frameworks in recently introduced polymers.
To evaluate the trueness and marginal fit of additively or subtractively manufactured polymer-based complete-arch implant-supported frameworks, comparing with those of strength gradient zirconia frameworks.
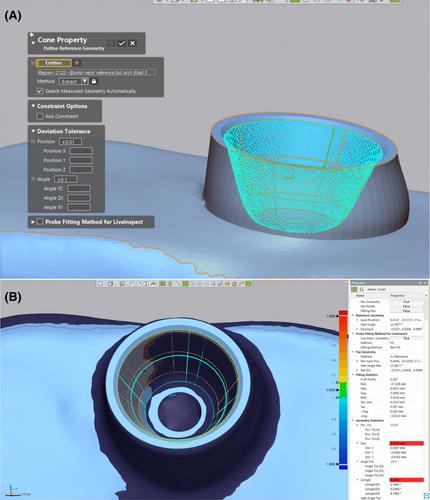
A typodont model with 4 implants (left first molar (abutment 1), left canine (abutment 2), right canine (abutment 3), and right first molar (abutment 4)) was digitized (ATOS Core 80 5MP) and an implant-supported complete-arch framework was designed. This design file was used to fabricate frameworks from 5 different materials: strength gradient zirconia (SM-ZR), high impact polymer composite (SM-CR), nanographene-reinforced PMMA (SM-GR), PMMA (SM-PM), and additively manufactured temporary resin (AM) (n = 10). These frameworks were digitized and each scan file was virtually segmented into 4 regions (abutments, occlusal, overall without occlusal, and overall). The surface deviations at these regions, and linear and interimplant distance deviations were evaluated (Geomagic Control X). Marginal gaps were evaluated according to triple-scan protocol after seating frameworks on the model with the 1-screw test. Data were statistically analyzed (α = 0.05).
Surface deviations of all regions differed among tested materials (p ≤ 0.001). AM frameworks mostly had surface deviations that were similar to or lower than those of other materials (p ≤ 0.031), except for the occlusal surface, where it mostly had higher deviations (p ≤ 0.013). Abutment 4 of SM-CR had higher linear deviations than abutment 2 (p = 0.025), and material type did not affect the linear deviations within abutments (p ≥ 0.171). Interimplant distance deviations differed within and among materials (p ≤ 0.017), except for those between abutments 1 and 2 among materials (p = 0.387). Marginal gaps of subtractively manufactured materials differed among abutments, while those of abutments 3 and 4 differed among materials (p ≤ 0.003). AM frameworks mostly had lower marginal gaps at abutments 3 and 4 (p ≤ 0.048).
Although there was no clear trend among tested materials for measured deviations, marginal gaps of additively manufactured resin were mostly lower than those of subtractively manufactured materials and did not differ among abutment sites. Nevertheless, the differences in measured deviations among materials were small and marginal gaps were within the previously reported acceptability thresholds.