Bile duct injury (BDI) repair surgery is usually associated with morbidity/mortality. The neutrophil-to-lymphocyte ratio (NLR) easily assesses a patient's inflammatory status. The study aims to determine the possible relationship between preoperative NLR (pNLR) with postoperative outcomes in BDI repair surgery.
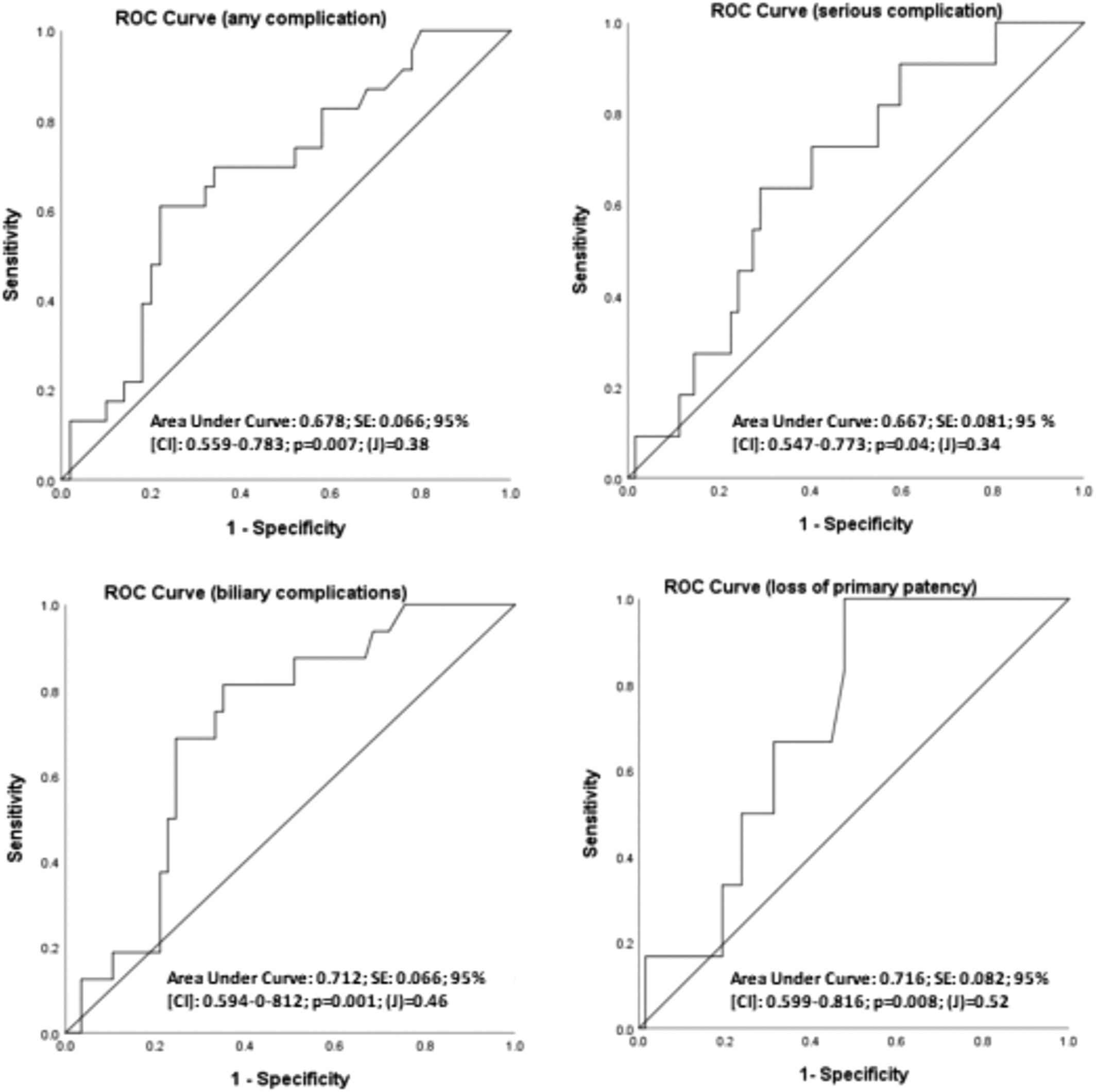
Approved Ethics/Research Committee retrospective study, in patients who had a Bismuth-Strasberg type E BDI repair (2008–2023). Data registered was: morbidity, mortality, and long-term outcomes (primary patency and loss of primary patency) (Kaplan–Meier). Group comparison (U Mann–Whitney), receiver operator characteristic (ROC): area under curve [AUC]; cut-off value, and Youden index [J], and logistic regression analysis were used for pNLR evaluation.
Seventy-three patients were studied. Mean age was 44.4 years. E2 was the commonest BDI (38.4%). Perioperative morbidity/mortality was 31.5% and 1.4%. Primary patency was 95.9%. 8.2% have lost primary patency (3-year actuarial patency: 85.3%). Median pNLR was higher in patients who had any complication (4.84 vs. 2.89 p = 0.015), biliary complications (5.29 vs. 2.86 p = 0.01), and patients with loss of primary patency (5.22 vs. 3.1 p = 0.08). AUC's, cut-off values and (J) were: any complication (0.678, pNLR = 4.3, J = 0.38, p = 0.007), serious complication (0.667, pNLR = 4.3, J = 0.34, p = 0.04), biliary complications (0.712, pNLR = 3.64, J = 0.46, p = 0.001), and loss of primary patency (0.716, pNLR = 3.24, J = 0.52, p = 0.008). Logistic regression was significant in any complication (Exp [B]: 0.1, p = 0.002), serious complications (Exp [B]: 0.2, p = 0.03), and biliary complications (Exp [B]: 8.1, p = 0.003).
pNLR is associated with complications in BDI repair with moderate to acceptable predictive capacity. pNLR could potentially predict patency of a BDI repair.