To investigate the differences in patient/caregiver characteristics, their treatment needs, and the attending physician's understanding of those treatment needs according to the duration after diagnosis of dementia with Lewy bodies (DLB).
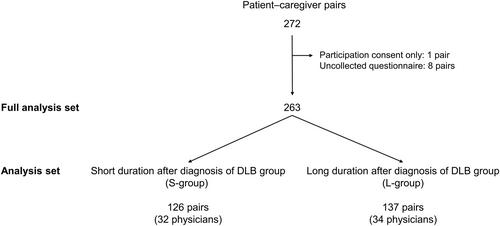
This was a post hoc analysis of a multicenter, cross-sectional, questionnaire survey study. A total of 263 patient–caregiver pairs were reclassified into two groups according to the median duration after diagnosis of DLB as follows: short (<24 months; S-group) and long (≥24 months; L-group) post-DLB diagnosis duration. Treatment need was defined as the symptom domain that caused the patient or caregiver the most distress. Concordance rates between patient–physician and caregiver–physician were calculated for physicians' understanding of treatment needs.
In this analysis, 126 pairs (32 physicians) and 137 pairs (34 physicians) were classified as the S- and L-groups, respectively. Patient and caregiver characteristics were broadly similar between groups (mean age for patients 78.7 ± 6.6 vs. 79.8 ± 6.7, for caregivers 64.7 ± 12.9 vs. 64.9 ± 12.8; number of male/female for patients 61/65 vs. 67/70, for caregivers 34/92 vs. 38/99), but the prevalence of parkinsonism (82.5% vs. 66.7%) and autonomic dysfunction (49.6% vs. 33.3%), severity of parkinsonism (MDS-UPDRS Part III total scores, 29.2 ± 22.6 vs. 18.0 ± 16.4; Part II total score, 14.6 ± 12.0 vs. 7.6 ± 7.9), and caregiver burden (J-ZBI_8 score, 9.1 ± 6.7 vs. 7.5 ± 5.8) were higher in the L-group than the S-group. Regarding treatment needs, the invalid answer rates for patients were 34.9% and 46.8%, and those for caregivers were 28.6% and 34.9% in the S- and L groups, respectively. Patients' treatment needs did not significantly differ (p = 0.056), but S-group patients were more likely to select cognitive impairment (p = 0.045) as their treatment need, whereas L-group patients were more likely to select parkinsonism (p = 0.003). Caregivers' treatment needs significantly differed (p = 0.032) between groups. S-group caregivers were more likely to select cognitive impairment (p = 0.001), whereas L-group caregivers were more likely to select other symptom domains such as parkinsonism (S-group vs. L-group: 10.3% vs. 16.7%), psychiatric symptoms (20.6% vs. 24.6%), sleep-related disorder (4.0% vs. 7.1%), and autonomic dysfunction (4.8% vs. 9.5%). Concordance rates between patient–physician and caregiver–physician were low in both groups.
There were some differences in characteristics according to the duration after diagnosis of DLB. Cognitive dysfunction may be a particular concern for patients and caregivers soon after diagnosis of DLB. Treatment needs of patients and caregivers for parkinsonism, psychiatric symptoms, sleep-related disorder, or autonomic dysfunction were different according to the duration after diagnosis of DLB. Physicians' perception of patients'/caregivers' treatment needs was poor regardless of the duration after diagnosis of DLB.
UMIN Clinical Trials Registry (UMIN000041844).