Patients with heart failure (HF) with improved ejection fraction (HFimpEF) may face residual risks of clinical events that are comparable to those experienced by patients with HF whose left ventricular ejection fraction (LVEF) has consistently been above 40%. However, little is known about the clinical course of patients with HFimpEF during hospitalization for HF.
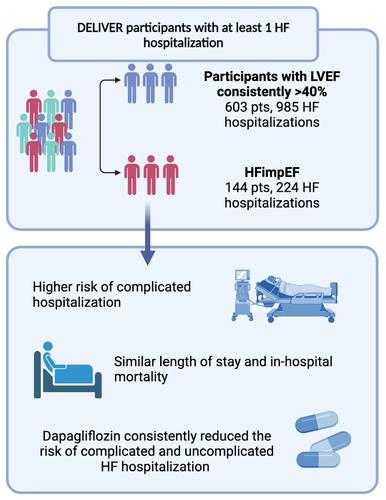
DELIVER randomized patients with HF and LVEF >40% to dapagliflozin or placebo, including HFimpEF (LVEF previously ≤40%). We evaluated all HF hospitalizations adjudicated by the clinical endpoints committee with available data for determination of in-hospital course. Complicated hospitalization was defined as any hospitalization requiring intensive care unit stay, intravenous vasopressors/inotropes/vasodilators, invasive or non-invasive ventilation, mechanical fluid removal, ultrafiltration, or mechanical circulatory support. LVEF changes were extracted using a validated GPT-3.5, a large language model, via a secure private endpoint. Of the 6263 patients enrolled in DELIVER, 1151 (18%) had HFimpEF. During a median follow-up of 2.3 years, there were 224 total HF hospitalizations in 144 patients with HFimpEF and 985 in 603 patients with LVEF consistently >40%. Patients with HFimpEF experienced higher rates of complicated HF hospitalization as compared with patients with LVEF consistently >40% (39% vs. 27%; p < 0.001). Among those who experienced a first HF hospitalization, there was no significant difference in length of stay or in-hospital mortality between patients with HFimpEF versus LVEF consistently >40%. In a subset of participants who had at least one LVEF measurement available during HF hospitalization, 66% of those with HFimpEF and 29% of patients with LVEF consistently >40% experienced a reduction in their LVEF to ≤40% from the time of enrolment (p < 0.001). In the entire DELIVER cohort, dapagliflozin reduced total uncomplicated and complicated HF hospitalizations, irrespective of HFimpEF status (pinteraction ≥0.30).
Among patients hospitalized for HF in DELIVER, those with HFimpEF experienced a more adverse in-hospital clinical course, necessitating higher resource utilization beyond standard diuretic therapy compared with patients with HF and LVEF consistently >40%, but had similar in-hospital mortality. Treatment benefits of dapagliflozin were not modified by hospitalization type.