Alcohol use disorder (AUD) is a multifaceted disease, and integration of AUD treatment between mental health and hepatology is necessary to improve outcomes. We aimed to ascertain whether patients with excessive alcohol use (EAU) and high FIB-4, which is a non-invasive method to identify advanced liver disease, are appropriately referred to hepatology and detect which clinical barriers, if any, might pertain.
Records of patients with excessive alcohol use between 2013 and 2023 were extracted from a large public system. Demographics, alcohol-related hospitalizations, mental health conditions, Charlson comorbidity index (CCI) and referral patterns were evaluated. Comparisons were made between those referred to hepatology versus not.
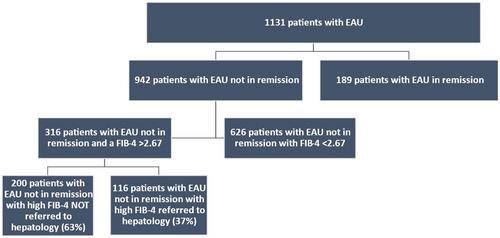
1131 subjects showed evidence of EAU but on further review, 189 were in alcohol-remission. The remaining 942 (636 men, age 55.7 ± 14.5 years, 548 white, 363 black, 19 Hispanic) subjects with CCI 2.61 ± 2.23 were further analyzed for FIB-4 score and referral patterns. 316 patients had active EAU and a high FIB-4, of whom only 116 (37%) were referred to hepatology. Patients with alcohol-related mental health concerns and admitted for trauma were less likely to be referred. Logistic regression showed referral was higher with alcohol-related liver hospitalizations (OR: 9.25, 95% CI: 4.90–17.47, p < 0.001), higher CCI (OR: 6.23, 95% CI: 3.00–12.94, p < 0.0001) and lower with mental health admissions (OR: 0.36, 95% CI: 0.15–0.48, p < 0.001) or mental health diagnoses (OR: 0.36, 95% CI: 0.15–0.82, p = 0.02) and increasing age (OR: 0.95, 95% CI: 0.92–0.97, p < 0.001).
In a large public health system, almost 63% of patients with EAU and FIB-4 >2.67 are not referred to hepatology for evaluation. Patients not referred were more likely to have alcohol-related mental-health hospitalizations and mental health diagnoses, while those with liver-related hospitalizations and comorbidities were more likely to be referred. Greater education of mental health providers and for teams taking care of inpatients admitted with alcohol-related mental health concerns would better integrate care and improve outcomes for patients with higher risk for advanced liver disease.