Sickle cell disease (SCD) is the most common hemoglobinopathy caused by an autosomal recessive genetic disorder leading to increased morbidity and mortality rates. SCD is prevalent in the Tharu community in the lowland (Terai) region of Nepal. Prevalence of metabolic syndrome among adults with SCD is poorly studied.
This prospective cross-sectional study was conducted at Seti Provincial Hospital in Dhangadhi, Nepal, among 140 adolescents and adults with SCD, aged 15–60 years. Anthropometric and laboratory data were collected using an assisted questionnaire, and the SPSS software version 23 was used for data analysis. Descriptive and inferential statistics were used to summarize the presence of metabolic syndrome and were stratified in separate analyses by age and sex. National Cholesterol Education Program-Adult Treatment Panel III criteria were used to define metabolic syndrome.
This cross-sectional study aimed to assess the prevalence of metabolic syndrome among SCD patients with SCD registered at the Seti Provincial Hospital in Dhangadhi, Nepal.
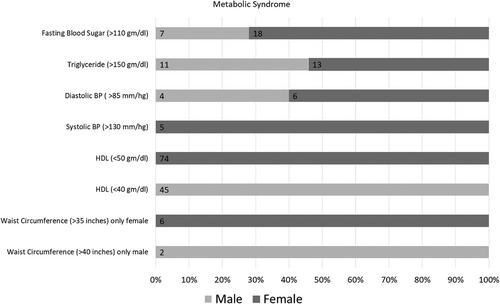
The prevalence of metabolic syndrome in the study participants was 7.8%. Our study revealed 5% of the patients overweight, and 1.4% obese. In this study, the mean triglyceride level was 118.5 mg/dL, and the mean high-density lipoprotein (HDL) level was 36.2 mg/dL (men) and 36.7 mg/dL (women). This study found that the mean fasting blood glucose level was 88.6 gm/dL. Similarly, 3.5% of patients had increased systolic blood pressure, and 7.8% had raised diastolic blood pressure. Study shows that changes in triglyceride level (p = 0.013), waist circumference, and HDL level (p = 0.0001 and 0.0048, respectively) are significantly associated with smoking or alcohol consumption; however, change in blood pressure (p = 0.013) and fasting blood sugar level (p = 0.086) are not associated with smoking or alcohol consumption.
Study concluded that though a lower proportion of SCD patients met the criteria for metabolic syndrome than in studies conducted in developed countries, it is crucial to consider metabolic syndrome while managing patients with SCD. Nevertheless, the authors advocate a more comprehensive study to draw significant conclusions.