Traditional fixed thresholds for oral glucose tolerance test (OGTT) results may inadequately prevent adverse pregnancy outcomes in twin pregnancies. This study explores latent OGTT patterns and their association with adverse outcomes.
This study retrospectively analyzed 2644 twin pregnancies using latent mixture models to identify glucose level patterns (high, HG; medium, MG; and low, LG) and their relationship with maternal/neonatal characteristics, gestational age at delivery, and adverse outcomes.
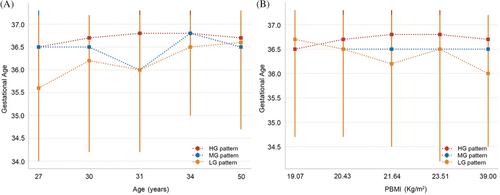
Three distinct glucose patterns, HG, MG, and LG patterns were identified. Among the participants, 16.3% were categorized in the HG pattern. After adjustment, compared with the LG pattern, the HG pattern was associated with a 1.79-fold, 1.66-fold, and 1.32-fold increased risk of stillbirth, neonatal respiratory distress, and neonatal hyperbilirubinemia, respectively. The risk of neonatal ICU admission for MG and HG patterns increased by 1.22 times and 1.32 times, respectively, compared with the LG pattern. As gestational weeks increase, although there is an overlap in the confidence intervals between the HG pattern and other patterns in the restricted cubic splines analysis, the trend suggests that pregnant women with the HG pattern are more likely to face risks of their newborns requiring neonatal intensive care unit admission, and adverse comprehensive outcomes, compared with other patterns. In addition, with age and body mass index increasing in HG mode, gestation weeks at delivery tend to be later than in other modes.
Distinct OGTT glucose patterns in twin pregnancies correlate with different risks of adverse perinatal outcomes. The HG pattern warrants closer glucose monitoring and targeted intervention.