Glioblastoma multiforme (GBM) poses a significant health challenge as the most common primary malignancy of the adult central nervous system. Gender- and age-related differences in GBM influence prognosis and treatment complexities. This multicenter retrospective study explores gender and age disparities in GBM patients, investigating their impact on occurrence and survival outcomes.
This multicenter retrospective study involved GBM patients treated in Guilan Province, Iran. Patients' data, including age, gender, tumor location, and histopathological diagnosis date, was collected from medical records.
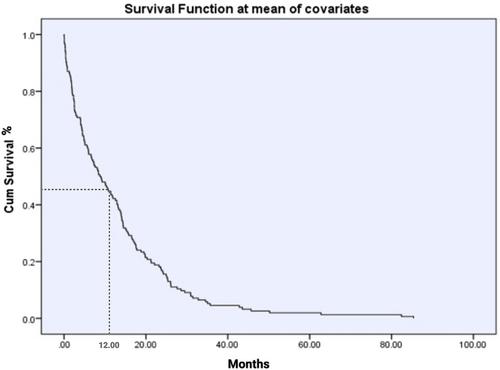
In a cohort of 164 GBM patients, the average age was 54.34 ± 14.16 years, with a higher prevalence among men (59.8%) and patients aged ≤ 60 years (64.6%). The tumor sites exhibited overlapping features in 68% of cases, with the frontal and temporal lobes being the most common specific locations. The mean survival was 12.88 ± 14.14 months, one-year survival of 45%, with women showing significantly higher one-year survival (60% vs. 40%) and longer mean survival (16.14 ± 17.35 vs. 10.75 ± 11.15 months). Furthermore, Patients ≤ 60 years had significantly higher one-year survival (75% vs. 35%). In subgroup analysis, women had significantly higher survival rates in patients ≤ 60 years. However, among patients over 60, women exhibited a more pronounced decline in survival rates, with no statistically significant difference between men and women in this age group.
This study highlights that both age and gender significantly affect GBM survival outcomes. Younger patients, particularly women, exhibited better survival rates, while older patients, especially women, showed poorer outcomes. These findings suggest the need to stratify treatment approaches by both age and gender to optimize care and improve survival in GBM patients. Further research is recommended to explore these associations.