Isolated vaginal vault recurrence of endometrial cancer can be treated with rescue radiotherapy. However, in previously irradiated patients, surgical resection can be considered the treatment of choice. Vesicovaginal fistulas (VVFs) sometimes complicate the surgical intervention because of the presence of massive ischemia and fibrosis of pelvic tissue from previous irradiation. Traditional strategies for the treatment of VVFs include endoscopic treatment (when feasible) or a laparoscopic, robotic, or open abdominal approach in some experiences through a transvesical route. The last approach can be associated with long inpatient hospital stays, postoperative complications, and failure, especially in obese patients. Our report proposes a conservative approach with prolonged catheterization and placement of nephrostomy tubes to treat a VVF with laser therapy of the fistula.
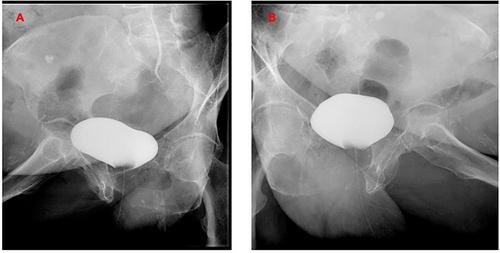
We present the case of a woman with a second relapse of endometrial cancer at the level of the vaginal vault, after a hysterectomy and then radiotherapy for a first relapse, who underwent robotic partial colpectomy, with an intraoperative bladder lesion, which was repaired with interrupted stitches. However, the patient developed a vesicovaginal fistula. A conservative approach was initially undertaken as an alternative to the surgical repair of the fistula. After the clinical and radiological confirmation of the fistula andconsidering the patient's clinical condition, the multidisciplinary team proposed a conservative management of the fistula as an alternative to fistula surgical repair. Bladder catheter Ch 20 and bilateral nephrostomy did not completely resolve the fistula, with a minor residual linkage between the bladder and the vaginal vault after 8 months from the robotic surgery. A single/month diode laser application for 3 months was added to the conservative treatment. Cystography was negative at the end of laser sessions, and both nephrostomies were removed 1 week later. After 6 months, clinical and radiological follow-up was negative, and no further vaginal urine loss was recorded.
We believe that conservative management of a complex vesicovaginal fistula after multiple treatments for endometrial cancer is possible. In this scenario, laser therapy can be a valuable clinical tool to improve the outcome, with reduced invasiveness for the patient.