HIV pre-exposure prophylaxis (PrEP) has been publicly available since 2018 in Australia as a daily regimen. In 2019, clinical guidelines were updated to support guidance on event-driven PrEP (ED-PrEP) use. We assessed trends in the PrEP dosing regimen by comparing daily PrEP use to ED-PrEP among cisgender gay, bisexual and other men who have sex with men (GBMSM).
Data from repeated, cross-sectional, national behavioural surveillance surveys were analysed from 2019 to 2023 among participants not living with HIV. Logistic regression models were conducted to assess trends and compared ED-PrEP users to non-PrEP users and daily PrEP.
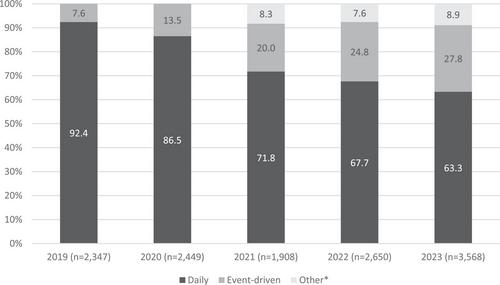
Among 38,880 participants, overall PrEP use with any regimen increased from 27.6% in 2019 to 42.7% in 2023 (OR = 1.16, 95% CI = 1.15−1.18, p < 0.001). Among 12,922 participants who reported PrEP use in the last 6 months, the proportion reporting ED-PrEP use increased from 7.6% in 2019 to 27.8% in 2023 (OR = 1.41, 95% CI = 1.37−1.46, p < 0.001) with those who reported daily PrEP decreasing from 92.4% to 63.3% (OR = 0.64, 95% CI = 0.62−0.66, p < 0.001). In a cross-sectional sub-sample in 2022–2023 (n = 8840), compared to ED-PrEP users, non-PrEP users were less likely to have received three or more HIV tests in the last 12 months (aRRR = 0.26, 95% CI = 0.22−0.31, p < 0.001), have 2−10 male sexual partners in the last 6 months (aRRR = 0.24, 95% CI = 0.14−0.41, p < 0.001) or 11 or more (aRRR = 0.26, 95% CI = 0.15−0.45, p < 0.001) compared to none, or to report condomless anal intercourse with casual partners (aRRR = 0.38, 95% CI = 0.32−0.46, p < 0.001). Compared to ED-PrEP users, daily PrEP users were more likely to have received three of more HIV tests in the last year (aRRR = 3.73, 95% CI = 3.15−4.40, p < 0.001) and less likely to be born overseas and lived in Australia for less than 5 years compared to being born in Australia (aRRR = 0.64, 95% CI = 0.49−0.83, p = 0.001).
While daily PrEP remains the most common PrEP dosing regimen among GBMSM in Australia, there has been a steep increase in the proportion of PrEP users who are taking ED-PrEP. Monitoring of PrEP use should continue to adapt to new dosing methods and future PrEP options. As ED-PrEP use increases, further work is needed to ensure those taking ED-PrEP are taking it effectively to prevent HIV.